Changes in Management of CLL Due to COVID-19 Noted in Italy
Changes in Management of CLL Due to COVID-19 Noted in Italy
This article was originally published by Cancer Therapy Advisor.
The clinical management of patients with chronic lymphocytic leukemia (CLL) was altered across Italy in response to the COVID-19 pandemic, according to a survey study published in Blood.
“What is starting to emerge is an impact on the routine work-up of patients, on treatment choices, and the enrollment and adherence to clinical trials,” the authors wrote.
The authors sent a survey to 33 hematology centers across Italy in early April that included questions about testing strategies for COVID-19; the effect of the pandemic on diagnosis, management, and the outcomes of patients with CLL; and the adherence to clinical protocols. The survey data was based on 9930 patients with CLL, which represents approximately one-third of all patients with CLL in Italy.
Although the minimum testing requirements mandated by law were followed by all centers, only 30% of centers tested asymptomatic patients without any known contact with a COVID-19 case prior to initiating CLL treatment. The authors said that this “reflects the higher capacity of some regional health systems to performed analyze nasopharyngeal swabs.”
CONTINUE READING
Of the 9330 patients with CLL, 47 (0.5%) patients were symptomatic and tested positive for COVID-19.
Most centers reported a decrease in the number of newly diagnosed CLL cases, likely due to a decrease in the use of peripheral laboratories for diagnostic work-up, the authors said. In addition, 15.2% of centers reported that delays and difficulties in an accurate diagnostic work-up has occurred due to a reduction in personnel.
New treatment initiation was delayed in 79% of centers, and 24% of centers reported a delay in ongoing therapy. Delayed post-treatment restaging also occurred in 30.3% of centers.
The sample size was not large enough to characterize patient outcomes due to COVID-19 or the effect of anti-CLL treatments. However, there was a mix of patients who were receiving active first-line or salvage treatment vs no active treatment.
The mortality rate in this cohort was 30.4%. “The mortality rate for symptomatic COVID-19 patients amongst the general population was 13.4% and 25.5% in the 70- to 79-year-old population,” the authors noted.
Clinical trial enrollment and follow-up of patients on a clinical trial protocol was reduced in two-thirds of the centers.
The authors concluded that this survey has revealed that COVID-19 “has started to impact on the number of new cases, on the adequate follow-up of treated patients, on the number of patients enrolled in clinical trials, and on the monitoring of such patients.”
Dr. Al-Sawaf on Fixed-Duration Versus Continuous Treatment in CLL
Dr. Al-Sawaf on Fixed-Duration Versus Continuous Treatment in CLL
This article was originally published by OncLive
Othman Al-Sawaf, MD, discusses benefits of a fixed duration treatment versus continuous treatment in chronic lymphocytic leukemia.
Othman Al-Sawaf, MD, a physician with the University Hospital of Cologne in Germany, discusses benefits of a fixed duration treatment versus continuous treatment in chronic lymphocytic leukemia (CLL).
Traditionally, patients with CLL have been treated with fixed-duration treatments, says Al-Sawaf. When chemoimmunotherapy was administered to patients, they usually received 6 cycles of treatment. As such, for approximately 6 months, patients would have to regularly visit the hospital for surgery, chemoimmunotherapy, or antibody infusions. However, most of the novel compounds that are emerging have been developed for continuous treatment that the patient can receive orally and until disease progression or unacceptable toxicity.
Therefore, the field started to move away from fixed-duration approaches to more tolerable, but continuously administered drugs, adds Al-Sawaf. Now, however, there has been a shift back to examining whether these novel compounds can be administered as a fixed-duration rather than continuous treatment, concludes Al-Sawaf.
Specialty Pharmacists Have Broad Responsibilities in Chronic Lymphocytic Leukemia
Specialty Pharmacists Have Broad Responsibilities in Chronic Lymphocytic Leukemia
This article was originally published by Pharmacy Times.
AT JUST 1.2%, chronic lymphocytic leukemia (CLL) represents a small percentage of all new cancer cases but is the most common leukemia in Western countries. In 2019, oncologists diagnosed an estimated 20,720 new cases and approximately 3930 people died. One virtual symposium held in conjunction with the Asembia Specialty Pharmacy Summit explored this cancer, which most often occurs in older adults.
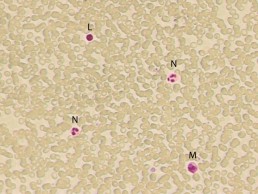
Alison Duffy, PharmD, BCOP, presented a comprehensive overview. Patients with CLL experience a gradual, malignant accumulation of lymphocytic blood cells that begins in the bone marrow and eventually extends to the blood. Genomic alterations cause leukemic transformation that inhibits apoptosis of clonal B cells. Del(17p) is the most important prognostic factor, reflecting the loss of a key tumor suppressor gene.
Oncologists generally begin treatment when patients’ end organ function is threatened, or they have progressive bulky disease, extensive adenopathy, or splenomegaly. Other factors that may signal a need for treatment are progressive bone marrow failure, constitutional symptoms, autoimmune anemia, leukostasis, or increasing absolute lymphocyte count. Those who are at least 65 years of age or who are younger and frail are treated in a “go slow” manner, whereas patients who are younger than 65 years with no significant comorbidities can be treated more aggressively.
Duffy discussed the evolving treatment paradigm of CLL, underscoring that therapy selection and patient management are complex. She focused on the small-molecule oral agents, including acalabrutinib, duvelisib, ibrutinib, idelalisib, and venetoclax, as well as evidence for their use in combination strategies. She demonstrated how each affects pathogenic pathways in CLL and also differentiated between treatment algorithms for naïve CLL and relapsed/refractory CLL. Ibrutinib and venetoclax are both approved as single agents in the first line, but other first-line therapies are combinations of acalabrutinib with obinutuzumab and venetoclax with obinutuzumab.
Duffy finished her presentation by discussing novel therapies currently in clinical trials and future implications. A number of other agents, both smallmolecules and monoclonal antibodies, are currently in clinical trials either alone or in combination with existing drugs.
Kirollos S. Hanna, PharmD, BCPS, BCOP, emphasized multidisciplinary collaboration with the fact that pharmacy-led chemotherapy management programs can improve 5 aspects of care:
- Patient knowledge
- Patient adherence to therapy and clinician adherence to prescribing standards
- Time to medication access
- Identification of clinically significant issues
- Provider and patient satisfaction
Hanna indicated that common standards of care exist for infection prophylaxis. He shared prophylactic recommendations for Pneumocystis jirovecii pneumonia, herpes simplex virus, cytomegalovirus, and hepatitis B related to use of specific agents.
Specialty pharmacists need to be closely involved with management of adverse effects (AEs). Hanna noted that AEs are the most common reason for kinase inhibitor discontinuation. He reviewed each agent’s most common AEs and suggested clinical interventions.
Hanna emphasized the importance of a medically integrated model. He discussed the 3 stages of treatment: (1) initiation, (2) coordination, and (3) maintenance, indicating that certain actions are “operational best practices.” A patient education checklist that he presented emphasized all of these points.
Finally, he highlighted the consequences of failure to access these costly agents. Prescription abandonment, poor adherence, treatment delay, decreased quality of life, and suboptimal disease outcomes are problematic for patients. He urged pharmacists to investigate benefits early in the process, have patients engage with assistance teams and counselors, look at every available co-pay assistance program, explore free drug programs, and integrate the financial team into the multidisciplinary process.
Discontinuation of Venetoclax Impacts Outcomes of Rituximab Combination in CLL
Discontinuation of Venetoclax Impacts Outcomes of Rituximab Combination in CLL
This story was originally published on Targeted Oncology
In an interview with Targeted Oncology, Anthony Mato, MD, discussed the findings of venetoclax interruptions or discontinuations observed in patients with relapsed/refractory chronic lymphocytic leukemia who received the combination of venetoclax plus rituximab in the phase 3 MURANO study.
Early discontinuation of venetoclax (Venclexta) was associated with suboptimal outcomes in an analysis of patients with relapsed/refractory chronic lymphocytic leukemia (CLL) in the phase 3 MURANO clinical trial, which was presented during the 2020 American Society of Clinical Oncology (ASCO) Virtual Scientific Program. These findings demonstrate the importance of effective management of adverse events (AEs) for patient to experience the full benefit of the combination venetoclax plus rituximab (Rituxan).
Discontinuation or dose interruptions of venetoclax appear to occur frequently in this patient population. This analysis aimed to evaluate how discontinuation or dose interruptions impact outcomes in this patient population.
Out of 194 patients, 140 completed 2 years of the combination regimen; 54 patients discontinued treatment early due to AEs in 29, disease progression in 12, withdrawal in 5, physician’s decision in 3, death in 2, noncompliance in 1, and for other reasons in 2. The median duration of venetoclax in patients who discontinued due to AEs was 11.3 months (range, 0.5-24.6) and 17.1 months (range, 4.6-25.1) for those who discontinued due to progressive disease (P =.08).
Inferior progression-free survival (PFS) was noted in patients who discontinued venetoclax early for any reason except for progressive disease or AEs compared with those who were able to complete treatment. Greater exposure to venetoclax cumulatively reduced the risk significantly of a PFS (HR, 0.93; 95% CI, 0.88-0.99; P =.0168) or overall survival (OS) event (HR, 0.85; 95% CI, 0.79-0.92; P =.0001).
Interruptions due to AEs occurred in 134 patients, which were mostly due to neutropenia (43%). The median duration of venetoclax interruptions was 9 days (range, 1-93). Interruptions did not have an impact on PFS or OS
In an interview with Targeted Oncology, Anthony Mato, MD, director of the Chronic Lymphocytic Leukemia Program, Memorial Sloan Kettering Cancer Center, discussed the findings of venetoclax interruptions or discontinuations observed in patients with relapsed/refractory CLL who received the combination of venetoclax plus rituximab in the phase 3 MURANO study.
TARGETED ONCOLOGY: Could you begin by providing some background on this study?
Mato: The MURANO trial is a trial comparing the combination of venetoclax and rituximab given for a total of 24 months, where the rituximab is given for 6 months and the venetoclax is given for a total of 2 years as compared to bendamustine/rituximab, which is a commonly used chemoimmunotherapy combination in the frontline and relapsed/refractory settings. The trial was conducted several years ago. Now we have 4 years follow up and initially and has subsequently demonstrated success in terms of the primary endpoint, in terms of PFS, as well as an OS advantage, favoring the venetoclax-based therapy, representing a paradigm shift in the management of patients with relapsed/refractory disease, in that we have a new molecule which rivals over a known standard of care, as well as a time-limited therapy approved in the relapsed/refractory setting.
TARGETED ONCOLOGY: Could you shed light on the methods that were used to conduct this particular analysis?
Mato: The analysis that was presented at the ASCO meeting is trying to address the question about whether or not outcomes are impacted for patients who have to undergo dose reductions, dose interruptions, and also for the small subset of patients who discontinue the time-limited therapy prior to the 24 months planned end point for continued therapy. Here we were looking at outcomes, particularly PFS, and how those particular factors might impact the primary end point of the MURANO trial for again, the small subset of patients who did require interruptions, reductions, and early or premature discontinuation.
TARGETED ONCOLOGY: What were some of the main reasons for discontinuing or interrupting treatment with venetoclax?
Mato: In most of the novel agents that have been approved for CLL, there’s always 2 competing factors that seem to lead to most of the dose reductions or interruptions and/or discontinuation, and those always seem to include AEs or progression of disease.
TARGETED ONCOLOGY: What do the results show in terms of the impact on outcomes?
Mato: The take home message from this trial is that it’s really best to try to understand how to use the label of venetoclax effectively to maintain continuous dosing for the 24 months. If patients required brief interruptions or dose reductions to try to find that right balance between AEs and continued exposure to this active agent, they were able to do just fine, and there was no significant impact on the outcomes. For patients who had to discontinue early, , those patients did have an impact on their outcomes. The lesson learned here is that if a patient requires a dose reduction due to neutropenia or diarrhea for example, it’s better to understand the label and appropriately apply supportive care and to dose reduce, rather than to just give up on using the combination all together.
TARGETED ONCOLOGY: Could you elaborate on what those supportive care measures would entail?
Mato: It depends on the AE. Frequently, in clinical practice, if a patient experiences neutropenia, for example, which is probably the most common AE, one can use growth factors like filgrastim (Neupogen) or pegfilgrastim (Neulasta) to support the white blood cell count. Fortunately, with venetoclax, you don’t need a lot of growth factor in order to maintain an absolute neutrophil count of about 1000, so sparing use once or twice a week might do it to maintain a dose of 400 mg. If the patient continues to experience neutropenia, then one might consider also reducing the dose from 400 mg, for example, to 300 mg or 200 mg. That might be 1 strategy.
Another supportive care measure is working with a clinical pharmacist to verify that there aren’t particular medication interactions that might increase the venetoclax dose or level such that you may experience AEs. Patients who have diarrhea, for example, might benefit from a brief hold, a dose reduction, a brief interruption, or use of supportive care. Like with any novel agent, there’s a learning curve associated with use of venetoclax, but once you’re able to understand the AEs, which are fairly predictable and it’s not like there’s hundreds of AEs associated with this drug, you can come up with measures related to dose reductions, interruptions, or adding in medications or supportive measures that allow patients to stay on drug.
TARGETED ONCOLOGY: Is there anything else you wanted to emphasize?
Mato: It’s important that these types of analyses are conducted when exploring the use of novel agents after the initial results of key trials are reported, particularly with the BTK inhibitors. We’ve seen similar types of analyses conducted, as well as less so with the Pi3K inhibitors, but I think it does provide an important framework for those practicing and taking care of patients who may require these types of measures in order to stay on drug to really help provide reassurance that outcomes are not compromised if you’re following the label and are able to stay on drug at a dose that’s right for a particular patient.
CLL Advocates NZ Newsletter Issue 1
CLL Advocates NZ Newsletter Issue 1
Welcome to our first CLL Advocates newsletter. Like many organisations, we weren’t able to accomplish very much over the lockdown period. We did, however, manage a Trustees’ teleconference to shape up our strategy for the next 12 months. One of the proposals made at that meeting was a monthly newsletter, so here is the first edition.
A huge number of lay and medical articles have been written about the COVID pandemic, and, as you may have seen on our website, we’ve published a number relevant to people living with CLL. See them here. One of particular interest was a consensus statement by Australasian haematologists on management of blood cancers in the COVID pandemic (published in May’s Internal Medicine Journal). It noted that, with a mean age of diagnosis of about 70 years, CLL patients are already likely to be in a high-risk group simply because of age. Advice specifically directed to CLL patients was:
- to delay planned therapy where possible
- to consider using oral agents over IV medications so as to avoid exposure to higher risk environments such as hospital chemotherapy units, for treatment of both initial therapy, and for relapsed/refractory disease (see our recent letter to Pharmac on this matter).
New Zealand has done extraordinarily well at this stage to contain the virus, though it should be noted that vaccination, if successfully developed, may present further challenges for CLL patients.
The CLLANZ Trustees’ meeting agreed that information/education initiatives on CLL should be high on our priority list. In this regard, a review of the current management of CLL by Dr Gillian Corbett, haematologist and trustee, has been published on our website. A detailed CLL patient information booklet is also now close to sign-off and will be published shortly.
In October this year we will be staging a half day or evening combined meeting/seminar on CLL in NZ with the Leukaemia & Blood Cancer (LBC) group, with leading NZ CLL specialists. This will be ‘in person’ in Auckland and also online on Zoom so that people from around the country can join in the discussion and if desired put questions to the speakers. Details will follow soon.
To ensure we reach as many people as possible who have an interest in CLL, we encourage you to become a ‘friend’ of CLL Advocates NZ – by signing up to our newsletter here and/or joining our private Facebook group. You can apply to join the group here.
More details of anticipated activities will follow in subsequent newsletters.
Meanwhile, now that we have passed the winter solstice, and are becoming adjusted to the new ‘normal’, stay well, physically, mentally and spiritually. And please remember that as well as our advocacy role, we want to be a source of knowledge and support for New Zealanders living with CLL, and their families and supporters. To help us achieve this we would welcome and appreciate your feedback, and your thoughts on how we can best achieve our mission.
With best wishes
Neil Graham FRACP, FRCP
Executive Director
CLL Advocates NZ
Three-Drug Combo Promising Against High-Risk CLL
Three-Drug Combo Promising Against High-Risk CLL
For patients with high-risk chronic lymphocytic leukemia (CLL), first-line therapy with a triple combination of targeted agents showed encouraging response rates in the phase 2 CLL2-GIVe trial.
Among 41 patients with untreated CLL bearing deleterious TP53 mutations and/or the 17p chromosomal deletion who received the GIVe regimen consisting of obinutuzumab (Gazyva), ibrutinib (Imbruvica), and venetoclax (Venclexta), the complete response rate at final restaging was 58. 5%, and 33 patients with a confirmed response were negative for minimal residual disease after a median follow-up of 18
Chemotherapy-Free Regimen Consisting of 3 Novel Agents for Previously Untreated, Poor Prognosis CLL
Chemotherapy-Free Regimen Consisting of 3 Novel Agents for Previously Untreated, Poor Prognosis CLL
Nearly 60% of evaluable patients with previously untreated, chronic lymphocytic leukemia (CLL) characterized by chromosomal deletion of 17p (del[17p]) and/or a deleterious TP53 mutation treated with obinutuzumab, ibrutinib, and venetoclax triplet therapy achieved either complete remission (CR) or a CR with incomplete recovery of the bone marrow, according to results of a single-arm, phase 2 study presented during the Virtual Edition of the 25th European Hematology Association (EHA) Annual Congress.
While less than 10% of patients diagnosed with CLL have disease characterized by del(17p), this biomarker is present in up to half of patients with refractory disease.2 Hence, there is an unmet need for efficacious and safe treatment regimens for this subgroup of patients. Furthermore, compounding this need is the finding that TP53 mutations, another biomarker of poor prognosis, have been reported to be present in approximately 90% of patients with disease characterized by del(17p) although only about 40% of those with TP53-mutant CLL also have del(17p).An unmutated IGHV gene is another risk factor for poor prognosis in the setting of CLL.2
Dr. Flinn on the Role of BTK Inhibitors in CLL
Dr. Flinn on the Role of BTK Inhibitors in CLL
This story was originally published on OneLive
Ian W. Flinn, MD, PhD, discusses the role of BTK inhibitors in chronic lymphocytic leukemia.
Ian W. Flinn, MD, PhD, director of the Blood Cancer Research Program, Sarah Cannon Research Institute, discusses the role of BTK inhibitors in chronic lymphocytic leukemia (CLL).
BTK inhibitors such as ibrutinib (Imbruvica), acalabrutinib (Calquence), and zanubrutinib (Brukinsa) have been transformative in the treatment of patients with B-cell malignancies such as CLL, mantle cell lymphoma, marginal zone lymphoma, and Waldenström’s macroglobulinemia, says Flinn.
In CLL specifically, BTK inhibitors have become a prominent frontline standard of care, adds Flinn.
Though, it is important to acknowledge that the toxicities that are associated with ibrutinib, including arthralgias, atrial fibrillation, and, though rare, significant bleeding, often lead to treatment discontinuation in patients with CLL.
'CLL flares’ reported after stopping ibrutinib
'CLL flares’ reported after stopping ibrutinib
Patients with ibrutinib-resistant CLL should remain on the BTK inhibitor until immediately before starting their next therapy, Australian haematologists have advised. In a Commentary article in Leukemia & Lymphoma, Dr Chloe Tang and Associate Professor Constantine Tam wrote that ‘CLL flares’ – accelerated CLL progression after ceasing ibrutinib – can be difficult to distinguish from …
Durable disease control achieved with BTKi salvage therapy in patients with CLL
Durable disease control achieved with BTKi salvage therapy in patients with CLL
Patients with chronic lymphocytic leukaemia (CLL) who progress on venetoclax can achieve durable disease control with Bruton tyrosine kinase inhibitor (BTKi) salvage therapy, new Australian research reveals. The study included 23 patients with refractory/relapsed CLL who received a BTKi (ibrutinib [n=21], zanubrutinib [n=2]) after ceasing the BCL2 inhibitor venetoclax due to progressive disease. After initiating …
To continue reading click here.