As a Cancer Patient, Will I Need an Extra Dose of a COVID-19 Vaccine?
As a Cancer Patient, Will I Need an Extra Dose of a COVID-19 Vaccine?
This article was originally posted on Patients Power
Individuals who are immunocompromised, including people with cancer, are wondering if they will need an additional dose of a COVID-19 vaccine to increase their level of protection against the coronavirus. The Advisory Committee on Immunization Practices (ACIP), which makes recommendations to the Centers for Disease Control and Prevention, met on July 22 to discuss this issue, among other topics. The meeting was a preliminary step in discussing the safety and effectiveness of additional vaccine doses before any new recommendations can be made.
When a person has cancer, there are two main reasons why they have an increased risk of infection: Either the disease itself or its treatment may cause suppression of the immune system. When this happens, a person may be considered immunocompromised. It is estimated that close to 3% of the U.S. population is immunocompromised, including those with solid tumors and blood cancers, people who have had organ or stem cell transplants, and those being treated with drugs that affect the immune system, including certain chemotherapy medications and corticosteroids.
While research indicates a very strong response to the COVID-19 vaccines in the general population, there is growing evidence that some people who are immunocompromised have a less robust immune response, even after they have been fully vaccinated.
Let’s review a bit. With rare exceptions, it is vital for everyone with cancer to get a COVID-19 vaccination as soon as they can, including those on most active treatments. Many experts at the ACIP meeting reemphasized the importance of vaccinations for people who are immunocompromised and further pointed out the key role of a “circle of protection” surrounding those who are immunocompromised consisting of other vaccinated individuals. It is important that all household members and others you are in close contact with are vaccinated.
CLL and Dermatology
CLL and Dermatology
Overview
More than a quarter of CLL patients experience skin issues. On Thursday, August 12th, at 2 pm PDT/5 pm EDT, join host Michele Nadeem-Baker and two doctors from The Ohio State University Comprehensive Cancer Center – The James: Jennifer Woyach, MD, hematologist/oncologist, and Brittany Dulmage, MD, a dermatologist specializing in oncodermatology, for a discussion about CLL and skin. How do skin concerns factor into CLL treatment decisions? What role can a dermatologist play on a patient’s care team? Join us for the answers to these questions and more.
Newsletter #13: Submission to Panel Reviewing Pharmac
Newsletter #13: Submission to Panel reviewing Pharmac
Dear Friends
Our major activity over the past month has been engaging with the independent Panel set up by the Government to review Pharmac. In addition to preparing a submission to the Panel, we were able to meet and present our submission to them in person, and we also attended a workshop for patient advocacy groups. See our submission here.
Fellow trustee Dr Ben Schrader, CLL specialist and Malahgan Institute Clinical Director Dr Rob Weinkove and I presented our case to the Panel, and together with the ensuing dialogue we felt it was a valuable and hopefully productive session. The workshop which was attended by all but one member of the Panel and around 16 patient advocacy groups, demonstrated a strong uniformity of depth and breadth of concerns by attendees on the failings of Pharmac regarding funding applications for medical treatment.
The key points we made there and in our submission were as follows:
- Dialogue between Pharmac and agencies making applications for funding is characterised by long delays, lack of feedback as to where a therapy is at in the funding consideration process, and lack of transparency. A much more open approach to dialogue is required.
- There are inefficiencies and blurred responsibilities in the structure and function of Pharmac, eg assessment and procurement need to be done by separate organisations.
- Funding is a major issue, both absolute budget, and the percentage of health budget NZ spends on medications compared to other OECD countries.
- Opinions of NZ consultants and specialist societies are rejected, as are international therapeutic guidelines put together by world authorities. There are examples, too, of the medical literature opinion being rejected as inadequate.
- There are examples of medications being widely available in other countries that are life-saving, and which Pharmac rejects funding thereof. This has resulted in people leaving NZ to get access to these life-saving medications. Case histories of such funding applications to Pharmac are available.
- Lack of funded international standard-of-care treatments in NZ also means we have very few clinical trials, a loss both for patients and clinicians.
- There are mechanisms for assessing how efficacious a drug is eg QALY, which should be a component of Pharmac’s decision process. Another component of non-funding of therapies is that those who can fund medications survive, and those who can’t don’t.
- Several attendees commented on “hidden” costs of treatment not being considered by Pharmac, such as the need to attend a tertiary hospital eg Day Stay Unit for treatment, which might involve long travel times for some people, the need to curtail employment, and the extra challenges that the elderly, disabled, and minorities such as Māori and rural living people face in accessing health care. Cancer Care at the Crossroads is an expansive guide to how oncological services in NZ should be.
- The consequences of successful treatment, such as returning to work as a fully functional member of society needs also to be factored into costs/savings.
- There are international models that function better re drug funding than Pharmac that Pharmac could transition into eg UK (NICE), Canada (CADTH),and Australia (PBAC).
- There have been major improvements in treatment options in oncology particularly over the last decade plus, but Pharmac’s response to these, often expensive, therapies has been anachronistic, and people are dying unnecessarily as a consequence.
- Vacillation has been a feature of serial decisions by Pharmac re grading of funding recommendations for medications. For an example of this see the final page of the submission on the history of Pharmac committee decisions over the past 6 years regarding ibrutinib.
- “Deeply frustrating“ has been an expression used to describe the interaction between funding application agencies and Pharmac.
The Review Panel will present its interim report to the Government on 16 August. We are of course awaiting this with great interest, and I will report to you again as soon as we’ve had an opportunity to digest it.
Best wishes

Neil Graham
Covid-19 Vaccines May Not Produce Sufficient Antibody Response in Transplant Recipients
COVID-19 Story Tip: Covid-19 Vaccines May Not Produce Sufficient Antibody Response in Transplant Recipients
This story was published on John Hopkins Medicine.
When clinical trials were conducted to determine the immunogenicity — the ability to elicit an immune response — for the first two vaccines marshaled against SARS-CoV-2the virus that causes COVID-19, one group was not among those included: people who have received solid organ transplants and others (such as those with autoimmune disorders) who are immunocompromised.
Now, Johns Hopkins Medicine researchers have tried to rectify that inequity, taking one of the first looks at how people who are immunocompromised respond to their first dose of one of the two mRNA vaccines — Moderna and Pfizer-BioNTech — currently being administered worldwide. Their findings, as published March 15, 2021, in a research letter in the Journal of the American Medical Association, disappointingly show that only 17% produced detectable antibodies against the SARS-CoV-2 virus.
“This is in stark contrast to people with healthy immune systems who are vaccinated, nearly all of whom mount a sufficient antibody defense against COVID-19,” says study lead author Brian Boyarsky, M.D., a surgery resident at the Johns Hopkins University School of Medicine.
The study evaluated the vaccine immunogenic response for 436 transplant recipients, none of whom had a prior diagnosis of COVID-19 or tested positively for SARS-CoV-2 antibodies. The median age was 55.9 years and 61% were women. Fifty-two percent were administered a single dose of the Pfizer-BioNTech vaccine and 48% received one shot of the Moderna vaccine. The median time since transplant for the participants was 6.2 years.
At a median time of 20 days after the first dose of vaccine, the researchers report that only 76 of the 436 participants (17%) had detectable antibodies to the SARS-CoV-2 virus. The researchers also found that among the 76 transplant recipients, the most likely to develop an antibody response were those younger than age 60 who did not take anti-metabolites for immunosuppression and who received the Moderna vaccine.
“Given these observations, we feel that the U.S. Centers for Disease Control and Prevention should update their new guidelines for vaccinated individuals to warn immunocompromised people that they still may be susceptible to COVID-19 after vaccination,” says study senior author Dorry Segev, M.D., Ph.D., the Marjory K. and Thomas Pozefsky Professor of Surgery and Epidemiology and director of the Epidemiology Research Group in Organ Transplantation at the Johns Hopkins University School of Medicine. “As the guidelines are currently written, people assume that vaccination means immunity.”
Segev says that upcoming studies will define the immunogenic response of organ transplant recipients and other immunocompromised patients after a second vaccine dose. Other studies will look at the impact of more extensive immune system profiling — including characterizing the immune cells that remember SARS-CoV-2 after vaccination and produce antibodies, or directly attack the virus in response to the presence of the virus — to help guide vaccination strategies for this population.
Boyarsky and Segev are available for interviews.
CLL Advocates Newsletter Issue 12
CLL Advocates Newsletter Issue 12
Dear Friends of CLLANZ
Covid-19 and CLL prevention and treatment – an update.
There is still a lot not known about this disease, but knowledge of it increases daily, and we will know a lot more about what to do to control the disease in coming months.
People who have CLL, and other leukaemias and blood cancers, are much more susceptible to the disease, have more severe disease, are more likely to be hospitalised when they get it, and are more likely to succumb to it than people with normal immune function.
Get vaccinated, if you have CLL.
Vaccination is safer than not being vaccinated – it reduces the severity of the disease, and the mortality rate, even though the vaccination response is reduced (it seems variably and complexly so) in people with CLL.
Herd immunity, nationally and globally, mainly because of vaccination, remains the mainstay of keeping people with CLL safe.
Preventative measures, such as avoiding crowds, social distancing, wearing protective gear such as masks, and washing hands, all remain important measures in preventing disease transmission.
And if you do get it, there seem to be increasingly recognised therapeutic options that can help you. For example, dexamethasone and budesonide save lives, and ibrutinib may reduce the disease severity.
Conversely, some treatments cause immunosuppression, and so increased vulnerability to the disease.
At the moment, in NZ, we have very low rates of the disease, and minimal community transmission, so we’re in a good place to be for staying safe.
This might change if the delta variant becomes established here though – it is more infectious, more likely to need to be treated in hospital, and maybe more resistant to vaccination, especially in the context where a person has only had one dose.
So I hope you all stay well during the pandemic out there in CLL land.
Best wishes

Neil Graham
Is there a link between CLL and stomach pain?
Is there a link between chronic lymphocytic leukemia and stomach pain?
This article was originally posted on Medical News Today
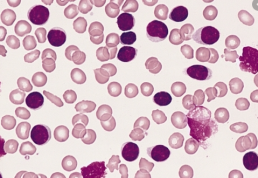
Chronic lymphocytic leukemia (CLL) is a type of blood cancer. It affects lymphocytes, a type of immature white blood cell that the body produces in the bone marrow.
People with CLL may experience discomfort, swelling, and pain in the abdomen if their spleen enlarges. In rare cases, CLL can also affect mucosal tissues, such as those lining the gastrointestinal (GI) tract.
This article discusses the link between CLL and stomach pain in more detail. It also looks at ways to prevent and treat CLL, the other possible symptoms, and the outlook for people with this condition.
People with CLL may experience various symptoms involving the abdomen or stomach, such as:
- discomfort, pain, or tenderness
- feeling full after eating small amounts of food
- swelling
- diarrhea or vomiting
- abdominal cramping
- loss of appetite
- unexplained weight loss
In most cases, people with CLL do not experience abdominal symptoms due to the disease until it progresses and becomes more severe.
Research suggests that CLL infiltrates and affects the GI tract in about 5.7–13% of cases. When CLL affects the GI tract, doctors may call it Richter’s syndrome.
People with CLL may experience abdominal swelling, discomfort, and tenderness as a result of their spleen becoming larger. Less commonly, they may also feel full after eating small amounts of food, as the spleen can press on the stomach, making it smaller and able to hold less.
In rare cases, CLL infiltrates the lining of the GI tract, causing inflammation and ulcers or open wounds. People may experience symptoms similar to those of inflammatory bowel disease (IBD) and malabsorption disorders. These symptoms may include diarrhea, nausea, vomiting, abdominal pain and cramping, and unintentional weight loss.
CLL is cancer that develops in lymphocytes, which are white blood cells that form in the bone marrow and help fight infection.
Lymphocytes make up most of the lymph tissues in the lymph nodes, thymus gland, adenoids, tonsils, and spleen. They are also present in the GI tract, bone marrow, and respiratory system.
CLL is a type of leukemia that develops gradually over time.
About 50–75% of people with CLL do not experience noticeable symptoms. Due to this, doctors diagnose most people with CLL during routine blood work.
The symptoms of CLL often begin when the cancerous cells crowd out healthy cells in the bone marrow or migrate to other organs or tissues. When symptoms first appear, they are typically mild, but they then become increasingly severe. CLL can cause many nonspecific symptoms, so a person may feel as though they have a cold or the flu.
Possible symptoms of CLL that do not relate to the abdominal area include:
- swollen lymph nodes
- frequent infections that are difficult to recover from
- unexplained exhaustion or weakness
- unexplained breathlessness or breathing issues
- excessive or abnormal bruising
- nosebleeds and heavy periods
- bone pain
- night sweats
- low grade fever
- jaundice, which is a yellowing of the mucous membranes, whites of the eyes, or skin
CLL Advocates Newsletter Issue 11
CLL Advocates Newsletter Issue 11
Dear Friends of CLLANZ
Skin infection (cellulitis) and CLL – a cautionary tale
Cellulitis is an infection of the skin, most commonly of the legs. It is usually due to bacteria. It commonly arises when the integrity of the skin is breached by a penetrating injury, often in the context of a pre-existing condition, such as diabetes, and conditions where immunity is impaired, such as CLL.
Cellulitis is the second most common primary site causing severe infection in patients with CLL (lower respiratory tract infections are the most common). It is often associated with sepsis/septicemia; when this happens, mortality is about 25% one month on from the episode of cellulitis. So awareness of what cellulitis is, and prompt antibiotic treatment thereof can save lives.
Professionally and theoretically, I have always been concerned about the risks of cellulitis, but in practice I’ve always led a physically active lifestyle, acquiring numerous skin injuries in the process. So it’s perhaps surprising that I hadn’t ever got cellulitis.
That all changed recently, when I had a penetrating injury of my left leg by a stick. Twelve hours later, I awoke in the night feeling very unwell, with a red, swollen, and painful leg. I was admitted to hospital for five days of intravenous antibiotics (blood cultures were positive for E. coli), with a good response, and was sent home on oral antibiotics.
About a week later, the infection recurred, despite oral antibiotics, and I again felt very unwell. I was readmitted to hospital, the first few days of this period being in ICU/HDU because of my level of unwellness. Blood cultures were again positive for E. coli. This time, I was an inpatient for a total of fifteen days; IV antibiotics for all that time, then a further week of IV antibiotics as an outpatient, after discharge. This seems to have done the trick, and I am currently back to where I was pre-leg injury, health-wise.
So, for those with CLL, please look after your skin, particularly on your legs. Wear gumboots and other protective clothing when in the outdoors, seek prompt medical advice/treatment for any skin injuries, and keep a careful eye on such injuries. Sepsis can be serious/fatal quite quickly.
I for one have certainly adopted a change in approach to looking after my skin as a consequence of this episode.
Best wishes

Neil Graham
Attempting to target the tumor microenvironment leads the way to an array of potential targetable pathways in the disease..
According to the researchers, attempting to target the tumor microenvironment leads the way to an array of potential targetable pathways in the disease, including through the use of combination therapy.
A variety of treatments spanning different treatment classes are being studied for use in chronic lymphocytic leukemia (CLL) in an attempt to target the tumor microenvironment environment (TME) of CLL, which attributes to the disease’s genetic complexity. In a recent review, researchers outlined the potential of the approach.
According to the researchers, attempting to target the TME, which is essential for the development, growth, and survival of malignant B-cell clone in CLL, leads the way to an array of potential targetable pathways in the disease, including through the use of combination therapy.
“It is becoming evident that improving clinical responses (residual and progressive disease), overcoming toxicity, infection risk, as well as drug resistance, likely require strategies aimed at reshaping the immunosubversive, pro-tumor TME state,” explained the researchers. “Our improved understanding of the direct and indirect CLL-TME modulations by novel therapeutic agents in recent years provides a unique opportunity to optimize CLL treatment with strategic drug combinations that target multiple CLL-TME interactions to achieve therapeutic synergy while controlling toxicity.”
Combinations include adding venetoclax to ibrutinib, which has showed promise for improving the duration of remissions, as well as adding the PI3K inhibitor duvelisib to venetoclax to improve the sensitivity of CLL cells. The latter is currently being tested in clinical trials.
Venetoclax has also showed promise in combination with anti-CD20 antibodies, with the combination demonstrating in vitro an improvement in the phagocytosis of CLL cells by macrophages while reversing resistance to venetoclax.
“Interestingly, although venetoclax plus anti-CD20 treatment produces impressive clinical responses in clinical trials, a recent retrospective study including real-world data demonstrated comparable efficacy between venetoclax as a single agent and venetoclax plus anti-CD20 combination treatment in high risk relapsed/refractory CLL patients,” wrote the researchers, “Thus, further validating prospective studies are warranted to determine whether the addition of an anti-CD20 antibody to venetoclax is truly necessary.”
On the other hand, adding an anti-CD20 antibody to ibrutinib also seemed to result in faster remissions and lower residual disease but was found to not improve profession-free survival.
This article was originally posted AJMC
Research has also focused on chimeric antigen receptor (CAR) T-cell therapy, as identifying treatment regimens that overcome T-cell dysfunction and improve the efficacy of T-cell-based treatments and immune checkpoint blockade represent some of the biggest challenges in CLL.
Early research has indicated that adding ibrutinib to CAR T-cell function concurrently may enhance CAR T-cell function. In one clinical pilot study, adding concurrent ibrutinib to CD19-targeted CAR T-cell therapy showed strong response rates in patients with relapsed/refractory CLL. The treatment combination also showed lower toxicities than CAR T-cell therapy alone.
Reference
Svanberg R, Janum S, Patten P, Ramsay A, Niemann C. Targeting the tumor microenvironment in chronic lymphocytic leukemia. Haematologica. Published online April 22, 20
Medical specialist says Pharmac 'wish list' is a 'necessity list'
Medical specialist says Pharmac 'wish list' is a 'necessity list'
Health expert discusses Pharmac’s funding option list
Watch the video here. Credits: The AM Show.
For the first time there is transparency with Pharmac.
The released ‘Options for Investment’ list, provided to Newshub, shows 73 medicines yet to be funded. Should the Government bite the bullet and invest in these life saving recommendations?
Former Executive Director of Association of Salaried Medical Specialists and health commentator Ian Powell joined The AM Show on Friday morning.
CLL Advocates Newsletter Issue 10
CLL Advocates Newsletter Issue 10
Dear Friends of CLLANZ
It was very interesting to learn in the news this week of Pharmac’s ‘wish list’ of 73 medicines it would like to pay for, if it had the budget to do so. It’s the first time Pharmac has released figures for what it calls its ‘options for investment’ list. The cost of funding them would be $417,670,000.00. Newshub got the story from an Official Information Act request – see it here, and see Pharmac’s formal response here.
The wish list is separated into proposals (118) and medicines (73), (as some medicines treat several illnesses) and it comes with a breakdown of how long they’ve been waiting. Although the list hasn’t been released, we expect Ibrutinib to be on it, as one of the 14 (of the total of 73) that have been waiting the longest, i.e. for 6+ years.
The timing of this is interesting, coming as it does in the lead-up to the Budget (May 20), and with Health Minister Andrew Little confirming to Newshub that any additional funding for Pharmac comes down to a political decision. That reality is also reflected in the government’s decision to exclude funding from the ‘independent’ review of Pharmac that is currently underway.
Filling the budget hole to fund the 73 ‘wish list’ medicines would mean a 40% increase in Pharmac’s funding, an increase that would go some way to bringing us into to line with Australia, the UK, Canada, etc. We don’t know what Pharmac’s bid has been for this year’s Budget, but last year they didn’t ask for any more money at all!
We in CLLANZ have worked hard over recent years through petitions, submissions, engaging with media, marching on Parliament, appearances at select committees, and actively engaging with Pharmac to advocate for access for CLL patients to Ibrutinib, among other treatments, as well as treatment pathway reforms, and faster, more transparent funding decisions. We’re very proud to have been part of the push to reform Pharmac, which is now seen as losing the PR battle.
We hope this work will bear fruit in the coming Budget, but in the meantime we intend to continue our advocacy as vigorously as possible. In this regard I warmly encourage you to support the current ‘Lie Down For Life’ campaign running nationwide on 12 May by Patient Voice Aotearoa. And if you haven’t already signed their petition to Reform Pharmac and Double its Budget, you can still do so here. This will be presented to Parliament on 12 May, the same day as we Lie Down For Life!
Kia kaha
Neil Graham