CLL and COVID-19: What Should Patients Know About Vaccines?
CLL and COVID-19: What Should Patients Know About Vaccines?
This article was originally published on Patient Power
What Vaccinations Should CLL Patients Receive?
With the flu season approaching and whispers of a vaccine for COVID-19 in the works, CLL patients with compromised immune systems may have questions about what vaccines they should be receiving, and if there are any risk factors involved. According to the experts, patients with CLL should schedule their flu shots right away, but what is recommended for a future COVID vaccine?
Listen in to find out more! Carol Preston, host and CLL patient advocate, will speak with Paolo Caimi, MD, Hematologist/Oncologist at University Hospital (UH) Cleveland Medical Center on these important topics.
In the Future, Should CLL Patients Get a Vaccine for COVID-19?
Carol Preston:
There is no vaccine at this time. We don’t know exactly when there will be a vaccine. And we know as CLL patients that we are only supposed to have dead vaccines as opposed to live viruses in a vaccine. So what is your thinking about a future COVID-19 vaccine.
Dr. Caimi:
What I am telling my patients is when the vaccine comes, we will first have to make sure that it’s safe. Second, I have to make sure that it’s safe for you. Meaning that for people with bad immune systems or people with half bad immune systems. Third, we’ll have to figure out with people who are less young, whether the dosing is different, whether the regimen is different. Then third, I’ll say probably what I’ll want them to do is to have everybody else around them vaccinated. Right?
So, in general, our patients are the ones who need to be beneficiaries of herd immunity, meaning everybody else’s immune to virus can’t touch them. And that’s probably what I would recommend them first to say, everybody else around you needs to be your barrier of protection for a vaccine. Once we figure out what the vaccine is going to be of benefit for you, maybe you need a different dosing, then we go ahead with it.
CLL Advocates NZ Newsletter Issue 6
CLL Advocates NZ Newsletter Issue 6
Friends of CLLANZ
Funding has been received, with thanks, from the BOP Medical Research Trust for a research project to be done as a summer studentship, by fifth year medical student, Andrew Weston, on “second primary malignancies in NZ CLL patients”.
Second primary malignancies are important in CLL, where the impaired immune system is not as able to deal to developing malignancies as people with normal immune systems can. As a consequence, about one third of CLL patients die of a second primary malignancy, such as melanoma, colon cancer, and pancreatic cancer. Some of these cancers have well-recognised screening procedures to detect early stage cancers, which can have a better outcomes to treatment then, compared to when they are picked up when symptoms develop.
Regular skin checks, and colonoscopy are two good examples of this screening approach.
I would be interested to hear from any of the CLLANZ Friends who are in this group i.e. have had a second primary malignancy, as it may help with the study.
I encourage you to spread the word about the existence of CLLANZ to any New Zealanders you know who are living with CLL, and encourage them to make contact with us.
The other request is to encourage you all to take an active approach to our Facebook group, and to continue to read HealthUnlocked and Patient Power newsletters , which are both easy groups to join, or can be read on our website.
A CLLANZ trustees meeting will be held this month, to review the year gone by, and to plan for the next twelve months. Please contact me at neil@clladvocates.nz to let me know about any topics you would like considered for the agenda.
Best wishes
Neil Graham
NICE recommends new chemo-free chronic lymphocytic leukaemia treatment
NICE recommends new chemo-free chronic lymphocytic leukaemia treatment
This article was originally published on EPR
The UK’s National Institute for Health and Care Excellence has recommended a new chemotherapy-free treatment for people with untreated chronic lymphocytic leukaemia (CLL). The institute said its recommendation of venetoclax plus obinutuzumab could benefit more than 1,000 people each year.
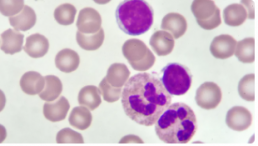
The innovative 12-month treatment will be offered to people with CLL who have not received any prior treatments. CLL affects white blood cells and is the most common chronic leukaemia, accounting for 30 percent of all adult leukaemias. In England there were 3,157 new cases of CLL in 2017.
Venetoclax plus obinutuzumab will be offered as a first-line treatment to people with CLL, with certain genetic abnormalities (such as a 17p deletion or TP53 mutation). For those without a 17p deletion or TP53 mutation, venetoclax plus obinutuzumab will be offered to patients with untreated CLL for whom fludarabine plus cyclophosphamide and rituximab (FCR) or bendamustine plus rituximab (BR) is unsuitable. The combination has also been made available via the UK’s Cancer Drugs Fund for this indication, so more evidence can be gathered on its cost effectiveness.
When and How CLL, SLL Should Be Treated
When and How CLL, SLL Should Be Treated
This article was originally published on Cure
Treatments for chronic lymphocytic leukemia (CLL) and small lymphocytic leukemia (SLL) have drastically improved in recent years, although patients may not need immediate treatment directly after being diagnosed.
Then, once it is decided that a patient will undergo treatment, deciding on the timing and regimen is pivotal.
When to Treat CLL/SLL
To determine if treatment is needed, patients should talk with their providers about symptoms they are experiencing, swollen lymph nodes, and blood cell counts, according to Dr. Locke J. Bryan, associate professor of medicine at the Medical College of Georgia and the hematology/oncology fellowship program director at the Georgia Cancer Center at Augusta University.
Bryan discussed CLL and SLL at the CURE® Educated Patient Leukemia & Lymphoma Summit.
One symptom of CLL and SLL is swollen lymph nodes; the location of the swelling could play a role in whether or not the disease is treated.
“It’s about location … a big node may not be causing any problems, but a smaller node pushing on an organ may cause some problems. Then, yes, the patient may need some treatment,” Bryan said. “And then as those (white blood cell) counts start to drop, that may be another reason.”
Dr. Awan on the Importance of Collaborative Care in CLL
Dr. Awan on the Importance of Collaborative Care in CLL
This article was originally published on Onc Live
The field of CLL continues to excel forward with novel molecular biomarkers, new therapeutic options, and ongoing clinical trials, says Awan.
Despite this, CLL remains a complex disease, Awan adds. As such, closely collaboration between community oncologists and CLL experts is often necessary to ensure patients receive optimal care.
Moreover, individuals who treat many cases of CLL may be able to recommend ongoing clinical trials that community oncologists are not aware of, Awan adds.
Ultimately, collaborative care is needed to identify new treatments and testing options, and to improve upon available therapies, Awan concludes.
Different Therapies and Modalities for Treatment of CLL in the Second Line
Different Therapies and Modalities for Treatment of CLL in the Second Line
This article was originally published on Targeted Oncology
During a Targeted Oncology Case Based Peer Perspectives event, Danielle Brander, MD, assistant professor of Medicine at Duke Cancer Institute in Durham, NC, discussed options for treating a 53-year-old female patients with chronic lymphocytic leukemia (CLL).
Targeted Oncology™: What are the guideline-recommended regimens to treat a patient with CLL such as this one?
BRANDER: The [National Comprehensive Cancer Network] guidelines for regimens in the relapsed/refractory setting include acalabrutinib [Calquence] and venetoclax [Venclexta], which are approved in all lines of therapy. In the relapsed/refractory setting, there’s also approval of duvelisib [Copiktra] and idelalisib [Zydelig], which are PI3K inhibitors.1
What data support the use of ibrutinib (Imbruvica), which is another guideline-recommended agent for the treatment of this patient?
The data that led to the initial approval of ibrutinib was the RESONATE trial [NCT01578707]. [The trial] randomized patients 1:1 to either ibrutinib or the anti-CD20 antibody standard-of-care agent in the relapsed/refractory setting, ofatumumab. Patients were allowed to cross over on this study.2
There are now 6-year follow-up data [showing that the] median progression-free survival [PFS] for the ibrutinib arm was not reached but was short [8.1 months] for the ofatumumab alone [HR, 0.133; 95% CI, 0.099-0.178].
Markers [of prognosis] that would indicate inferior response to chemoimmunotherapy are either the patients with IGHV unmutated or del(17p) or del(11q), who are still having good responses. This is in the relapsed/refractory setting with novel agents.
The grade 3 or greater AEs [adverse effects] that you’ll see are infectious complications. Infections and neutropenia do get better in terms of incidence with [time]. But obviously, if they have to stop [treatment] in the first year, it’s still detrimental to them. One thing [to keep in mind when] monitoring patients is that time on therapy does increase risks for hypertension. Atrial fibrillation and bleeding remain a risk throughout treatment. Often, they first appear early on treatment.
CLL Advocates NZ Newsletter Issue 5
CLL Advocates NZ Newsletter Issue 5
Friends of CLL Advocates NZ
I’m pleased to report on a very successful inaugural CLLANZ seminar on 14 October, co-hosted by LBC. Around 100 people attended either by zoom or in person in LBC offices up and down the country. There were three excellent presentations by three of NZ’s most authoritative clinicians on CLL. Dr Peter Browett described the disease, Dr Gillian Corbett spoke on therapy, and Dr Rob Weinkove explained likely future directions for CLL treatment. An informative panel discussion and questions session concluded the two-hour event.
I thank all those who helped organise and manage this event, and particularly LBC for providing their facilities. This will hopefully be the first of many such events in years to come.
The seminar has provided us with an up-to-date, comprehensive patient resource on CLL in NZ. A video of the full event will shortly be posted on our website, and the presentations can be found here.
Identifying the priorities we should be pushing for in CLL treatment was a key theme of the event. These included having testing available in NZ for IgVH mutations, and I’m pleased to say this has already stimulated momentum to develop this.
As well as being our inaugural seminar the event was the formal launch of CLLANZ, almost two years after we first discussed the idea of starting the group, somewhat delayed by COVID 19.
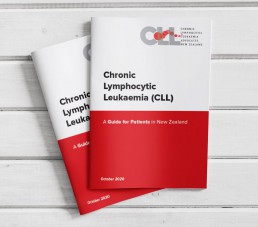
It was also the formal launch of our booklet “CLL – A Guide for Patients in NZ”. Again, dedicated individual and team effort resulted in an excellent, informative document, which is available here on our website and in hard copy. If you would like a hard copy please send us your postal address. The booklet is also being distributed to CLL clinics around NZ, where you can also pick up a copy. Feedback on this is welcomed.
We’ve already had a lot of positive feedback on the event, along with suggestions for future seminar themes, and would welcome further thoughts on this.
Best wishes
Neil Graham
Novel Prognostic Model Predictive of Survival in Ibrutinib-Treated CLL
Novel Prognostic Model Predictive of Survival in Ibrutinib-Treated Chronic Lymphocytic Leukemia
This article was originally published by Hematology Advisor
A 4-factor prognostic model may help to identify patients with chronic lymphocytic leukemia (CLL) at risk of ibrutinib failure, according to research published in the Journal of Clinical Oncology.
As CLL is a “clonal expansion of mature B cells drive by constitutive activation of B-cell receptor (BCR) signaling,” previous studies suggest that the selective inhibition of BCR and BCL-2 protein may significantly improve outcomes in some patients with CLL compared with chemotherapy as a first-line therapy.
Ibrutinib, a Bruton tyrosine kinase inhibitor, is frequently used in the CLL setting, though drug resistance invariably evolves, with relapse occurring often with ibrutinib monotherapy.
Identifying those at risk of relapse after ibrutinib therapy would improve treatment decision-making among patients with CLL. While there are existing prognostic indices, none specifically evaluate for criteria known to be linked with the evolution of ibrutinib resistance. In the present study, the researchers evaluated and validated the effectiveness of a 4-factor prognostic model among patients with CLL treated with ibrutinib.
CLL Advocates NZ Launches a New Zealand Patient Guide
CLL Advocates NZ Launches a New Zealand Patient Guide
CLL Advocates NZ is pleased to announce the official launch of its patient booklet, CLL – A Guide for Patients in New Zealand. It has been made available in both a digital download and as a hardcopy booklet.
The booklet is being launched at CLL Advocates NZ’s inaugural patient seminar in Auckland and online tonight (14 October). The seminar will discuss ‘What is the state-of-the-art treatment for CLL in New Zealand?’
The booklet was compiled by Leukaemia Care, a national UK blood cancer support charity. Leukaemia Care has kindly granted us permission to adapt the booklet for the New Zealand CLL setting, and to publish it here on our website, and make it available as a printed booklet for distribution in New Zealand. This agreement is in line with CLL Advocates NZ’s commitment to working closely with other CLL patient advocacy groups and to avoid duplicating available high quality work undertaken by others.
Adaptation of the booklet for New Zealand conditions has been undertaken by Gillian Corbett MBChB, FRACPath, MRCP, FRACP, haematologist and Trustee, CLL Advocates NZ, Neil Graham FRACP, FRCP, Executive Director, CLL Advocates NZ, and Catherine Isaac, Trustee, CLL Advocates NZ.
We are most grateful to Leukaemia Care for this very valuable contribution to our work.
To learn more about the booklet, download it, or to request a hardcopy click here.
Dr. Davids on Factors to Inform Treatment Selection in CLL
Dr. Davids on Factors to Inform Treatment Selection in CLL
This article was originally published by OncLive
Matthew S. Davids, MD, MMSc, director of clinical research in the Lymphoma Program and a medical oncologist with Dana-Farber Cancer Institute, as well as an assistant professor of medicine at Harvard Medical School, discusses factors to consider when selecting treatment for patients with chronic lymphocytic leukemia (CLL).
When deciding which modality to select for patients with CLL, comorbidities must be considered, says Davids. For example, if there is a patient with significant cardiovascular disease, particularly if he/she is on an anticoagulation medication for atrial fibrillation, BTK inhibitors may not be the optimal choice. For this patient, a venetoclax (Venclexta)-based regimen should be considered, according to Davids.
On the other hand, if a patient has poor renal function and tumor lysis risk is a concern or if he/she is older and has difficulty commuting to the medical center for frequent monitoring, then a BTK inhibitor is favored, says Davids. With this approach, there is less risk of tumor lysis and patients require less monitoring than they would with a venetoclax-based regimen, concludes Davids.