CLLANZ calls for home-based treatment for CLL patients during COVID pandemic
CLLANZ calls for home-based treatment for CLL patients during COVID pandemic
Last week CLL Advocates New Zealand wrote to Pharmac requesting them to provide temporary access to ibrutininb (taken in tablet form at home) for del17p and RR patients, and for newly diagnosed fit and unfit patients.
Read the letter below or download the letter here.
—
Dear Peter Murray, Deputy Medical Director
Thanks for your email clarifying the nature of changes Pharmac has made under Special Authority with respect to the management of cancer medicines, in light of the current COVID-19 crisis.
You have asked if I have any ideas on this issue that I would like to put forward for consideration and indeed I do. They concern risks posed by aspects of the current treatment of patients with CLL, as follows.
- A fellow Trustee of CLL Advocates NZ (CLLANZ), haematologist Gillian Corbett, has raised serious concern about the risks posed to patients in the administration of the current funded standard-of-care treatment for patients with del17p and relapsed refractory CLL. She has a patient starting treatment this week who had to go across town for urgent lab testing twice in one day, and again the following morning for tumour lysis syndrome (TLS) management. She noted that IV hydration needs to be considered in these patients, and that her patient will likely need to have more urgent blood tests during the coming week. She will need to have the procedure repeated next week. Gillian is very concerned about patients like this one having to put themselves at risk by going to the labs where there is likely to be a long wait, which in their immune-suppressed state would increase their risk of infection, including COVID-19.
For this reason we would like to propose that a change to CLL treatment be made under Special Authority to enable ibrutinib, which is taken in tablet form at home, to be funded temporarily for del17p and relapsed refractory CLL patients. In addition to being a home-based treatment, ibrutininb requires very little monitoring, infrequent blood tests and infrequent attendance at hospital (outpatients).
- We also propose that the Special Authority enables newly diagnosed fit and unfit patients to access ibrutinib, to avoid the need for chemotherapy or a delay in initial treatment. Again this would be a temporary SA to be in place until such time as patients can safely undergo in-hospital care.
- Finally we propose that the Special Authority for ibrutininb should also apply to treatment for CLL patients who are having intravenous therapy in a hospital setting, such as rituximab or obinutuzumab, which is given by infusion and requires, particularly initially, prolonged attendance at the chemotherapy department which is highly undesirable at this time of the COVID-19 epidemic.
As you would know, patients with CLL are immuno-compromised, and most are in the most at-risk age group, so we believe for all these reasons Pharmac should move quickly to make these changes.
I don’t have an accurate understanding of the numbers of patients this would involve, and I’m currently canvasing CLLANZ subscribers for further input on this issue. But I understand there has been a significant drop in people presenting with CLL, no doubt due to the general pattern of people avoiding going to the doctor. The same may be true of RR patients. I understand that HSANZ may be looking at the likely number of patients who would benefit from these changes, but that the numbers involved are likely to be very small and the costs therefore low.
It seems to me, at a time when so much effort is going in to saving lives, implementing this proposal would be a most worthwhile contribution from Pharmac.
I’d be very happy to discuss this with you or provide any further information you may require, and look forward to hearing back from you on this request.
Kind regards
Neil Graham FRACP, FRCP
Executive Director
CLL Advocates NZ
How it feels to be in intensive care with COVID-19 - a survivor with CLL
Coronavirus: This is how it feels to be in intensive care with COVID-19 - a survivor's graphic story
Robin Bowler, a lottery and gaming consultant, feared he’d never see his kids again after contracting coronavirus and ending up in intensive care – but a voice in his head somehow got him through.
This is a story of hope, his story – a survivor’s story:
If you were to write down the classic set of conditions that a single person may have, in which COVID-19 could thrive, you would probably end up with a profile that looked remarkably like me.
I am 58, I have asthma, I have one of those much-mentioned “underlying health conditions” – namely chronic lymphocytic leukaemia (CLL) – I am blood group A (reportedly more susceptible to the more aggressive form of coronavirus, with a high proportional death rate), and until recently, drank more than I should.
On the plus side, I happen to have a good level of underlying fitness and spend a lot of time outdoors.
So that’s me. Well, almost.
I returned from Italy on 7 March and first began to feel some slight chestiness during the evening of Monday 9th. Following a call with 111 I was recommended for a COVID-19 test, which was done on the 13th and I received confirmation from Public Health England by telephone the following Tuesday 17 March.
In the meantime my previously mild condition had turned for the worse into flu-like symptoms, and I could feel an infection growing in my chest.
By the Thursday night I was having serious problems breathing. So at 5am on Friday 20 March I called 111 again and was hospitalised that morning in an isolation room in the Lulworth ward of Dorset County Hospital.
Incredibly, at this time I did not feel particularly frightened, although the enormity of my decision to go to Italy was dawning on me – as was the realisation that if this got really serious, I was on my own.
There would be no family to visit, no contact with NHS staff other than that which was essential, an intercom to speak to front-line staff safely. Just me and the four walls of my room and its contents.
By Sunday 22 March it was clear that the committed care I was receiving from the doctors and nursing staff on Lulworth ward was simply not working.
A second chest X-ray revealed that what had been originally described to me as a “pneumonia” had worsened, my temperature spikes were climbing dangerously close to the 40C mark on multiple occasions, and I was weakening by the hour.
At this time, what was really bothering me was the fact that there had been a suggestion that they would send me home within a day, and I knew that I would not cope without the specialist care available within the hospital.
My concern levels rose to full anxiety and therefore late that afternoon I asked to speak with a doctor and, during a dialogue in which I became very emotional, he calmly reassured me that there was no way I would be sent home against my wishes, and that they would not consider discharge unless they were sure I was safe.
Shortly afterwards, I was visited by a senior consultant who I believe introduced himself as head of critical care at DCH.
He informed me that, having reviewed my situation, the decision had been taken to move me to intensive care as a precautionary measure, warning me in no uncertain terms that this was going to be a long haul.
He then fixed me with a hard look and added: “You may not survive this.”
I responded (equally calmly, I think): “I’ll do what I have to do.”
But inside, I could feel my confidence crumbling, my fear rising to hitherto unknown levels, and my mind starting to run amok with self-recrimination, longing to be with my (adult) children Natasha (Tash) and Luke, and a new sense that I had moved from a virus into a life-threatening situation which my combination of “underlying health conditions” just may not be able to cope with.
Within less than half an hour I was in intensive care, isolated in a room that looked like it was normally the area where staff monitored patients from. I had never felt so alone in all my life.
By midnight, I was busily convincing myself that I could well be dying and it was all my own fault. The thought of never seeing Tash or Luke again was simply unbearable, but in my mind and in fact, this was a realistic scenario that now existed.
I was being monitored by a team led by a senior consultant anaesthetist, who was asking me if I thought I could continue with the oxygen supply through my nose as a preferable alternative to full anaesthesia, intubation and being placed on a ventilator for an indefinite period of time.
Going onto a ventilator meant replacing my lungs with a mechanical breathing apparatus while disabling all my normal involuntary muscular activity involved with breathing.
After an hour I realised two things: firstly that my mental capacity to make what amounted to life and death decisions was by now seriously impaired and that I was incapable of making good decisions; and secondly that I was haunted by the fact that the second X-ray had been worse than the first, and so I was convinced that the current oxygen treatment was similarly not up to the job.
By 2am the decision was taken to “put me to sleep” and in a strange way I welcomed the ability to surrender all decision-making to these cool-headed, professional experts who knew much better than I did the risks I faced and trade-offs that were involved.
The process of being “put to sleep” was terrifying.
I was surrounded by medical staff, each with their own responsibility in the process, and all calmly and clearly directed by the senior consultant anaesthetist, who was pressing a face mask down on to my face with a force that made me feel that I could no longer breathe, while verbally reassuring me I was safe and would be taken very good care of.
I thought at the time that this could be the last I see of this life, and at the suggestion of the anaesthetist, thought of Tash and Luke for all I was worth, after which I remember nothing more of that night.
As it turned out, I was on the ventilator for approximately 36 hours during which time I remember nothing, but during which time I was kept alive by the skill of the medical teams and their sophisticated machinery.
I was brought out of the anaesthetic late afternoon on Tuesday 24 March and extubated (taken off the ventilator), and I can remember waking up, seeing blue sky through a window, and thinking “I’m still alive”. I was in the high-dependency unit by this time, and just the presence of natural daylight had the most profoundly positive effect upon me.
My immediate thought was to get a message to Tash and Luke that I was conscious again and I made that request (almost certainly in much more garbled form than I credited myself with at the time) which was duly granted.
The other feeling I had immediately was that I felt less exhausted than I had been that Sunday night, and much more ready for the prolonged fight ahead.
I was on oxygen support for the rest of Tuesday 24th, overnight and into Wednesday 25 March.
By this time I was coughing up thick globules of blood and sputum which had accumulated in my bronchus as a result of the intubation.
This was a serious problem, because every time I coughed this horrible stuff up, it made me vomit as well, which was thoroughly interruptive of the oxygen supply which was so essential to my survival at this point; and for the medical staff because it exposed them to more pure COVID-19 infectious material.
To give an idea of how sick I was at this time, one indicator called CRP (C-reactive Protein) showed that my reading was 340, where a non-infected person’s score should be minus 2.
My temperature was continuing to spike around the 40C mark (the point at which multiple organ failure can begin to set in), my blood saturation levels were poor, my blood pressure was “through the roof” (quote, unquote), and just about every other data point was out of whack.
Despite 36 hours on the ventilator, the virus was rampant within my body, particularly my lungs, and it was highly questionable whether I would make it through or not, with all my in-built disadvantages.
During the afternoon of Wednesday 25 March the team of consultants and doctors who were making collaborative decisions every hour made the decision to place me on CPAP support (continuous positive airway pressure) for however long may be necessary.
This involved a very tight-fitting face mask, through which a constant stream of pure oxygen is pumped directly into the lungs – in my case starting at 55 litres per hour.
I had two main concerns at this point: first, to keep breathing, and second, to try to suppress the coughing up of blood and sputum as I had no way of expelling it – the doctors told me I had to swallow it.
This was appalling to me, so we hit upon a compromise where I could use a thin suction tube to slide inside the CPAP mask without interrupting the flow of oxygen. This was more difficult and less practical than it sounds, and I soon found myself forcing myself to swallow the foul stuff, as I had been directed to. I was reminded of my defiant response “I’ll do what I have to do”.
Once the CPAP was started, I was on all sorts of medication. I had multiple cannulas in both arms, one in an artery, and one in my neck which allowed fluids to be poured down the back of my throat into my stomach – the water was okay, but the potassium was horrible.
But one of the medications was to reduce my level of anxiety, and so for the next 48 hours I became quite hallucinogenic as my mind was eased away from the drama of my situation, and so it started to float freely and at times bizarrely in all manner of directions.
During this 48-hour period, I found myself conversing with unknown others in a range of different accents from around the United Kingdom. Broad Scots, Northern Irish, Welsh, Geordie, Scouse, Cockney, Cornish – it was like taking a virtual tour of the UK and chatting with very amenable strangers who were full of good advice and encouragement.
And at times I would slowly descend into a sunny glade where people were relaxing, and as I got close enough to them to begin to discern their features, they vanished as quickly as they had appeared.
Other times I was floating in a circular motion inside a large natural bowl of thick green vegetation, but try as I might, I could never see the rim of the bowl and the sky above.
And all this time, the constant refrain of WHOOSH, HISS, WHOOSH, HISS, WHOOSH, HISS, dominating the weird version of consciousness that I found myself in. And a clear voice in my head then reminded me that I was fighting for my life.
It said that I was in the Staying Alive Factory, and that if I wanted to survive, I needed to stay on this noisy, uncomfortable, frightening production line; and that alternatively, if I fell off the production line, I would not make it through. So that was it.
Then the voice reminded me that I had a lot of explaining to do to Tash and Luke, and so I resolved there and then to remain on the production line – “I’ll do what I have to do”.
After approximately 48 hours on the CPAP, the same head of critical care came and asked how my breathing was.
The anti-anxiety medication must have been reduced or stopped by this time, because I clearly remember the conversation.
“Mmmch bttr,” came my reply.
“Sorry, did you say your breathing feels better?” repeated the doctor.
“Much better,” I forced out through the oxygen flow, the tight-fitting CPAP mask, and my by now completely dry mouth, throat and tongue.
I also felt instinctively that the industrial strength antibiotics they had been pumping through my body for days had finally got on top of the vicious bacterial infection in my lungs.
I had stayed on the production line, and I suddenly knew I could get past this. I could breathe to a depth that felt like it was self-sustaining (not actually quite the case at the time), and during the last few hours on the CPAP, I began to communicate by writing short notes on a clipboard given to me by one of the doctors.
One of the first notes I wrote was the question: when can I eat and drink something?
Within what seemed like a couple of hours, the CPAP was removed and replaced with a much gentler oxygen supply through my nose.
The instant calm that descended with the removal of the WHOOSH, HISS tyranny made me think I had moved from the main production line of the Staying Alive Factory to the body shop where, instead of destroying bad things and building back up good things, the focus moved to refined monitoring of what my body was able to do for itself again.
It was a beautiful day outside, that I could see from my bed. And it was a beautiful day inside my head, as I contemplated that I maybe would be seeing Tash and Luke again, and that my time had not yet come.
The rest, as they say, is history.
I was moved to Moreton ward, a convalescence ward where I was weaned off the oxygen supplies, given regular meals, and the recovery physio began. I was declared medically fit for discharge on Wednesday 1 April (an auspicious day if ever there was one), and I was reminded what a fool I’d been to play fast and loose with my health just to go on a skiing holiday. A mistake I will never make again.
Of course, there is no such thing as the Staying Alive Factory, which was an invention of my befuddled mind at a time of extreme health crisis.
What there is is the dedicated expertise, courage and commitment of the consultants, doctors, nurses, physios, Ancillary staff, and undoubtedly many, many others, of the NHS who collectively saved my life.
It may feel like a factory when you are undergoing such intensive care, but the key word here is care. It is to that care that I owe my life, and I will be forever grateful.
Originally published on Sky News
New Score Predicts When Patients With CLL Should Start Treatment
New Score Predicts When Patients With CLL Should Start Treatment
Most patients with chronic lymphocytic leukemia (CLL) are diagnosed with early stage disease and are managed with active surveillance, but there is much uncertainty over when to start treatment. A simple prognostic model, based on the sum of three routine tests, can now help with this decision, say researchers.
The new score is effective in predicting the amount of time a patient with CLL will likely have before requiring treatment, the team notes. “Other prognostic scores that are available mostly aim at predicting overall survival of patients who are in need of therapy,” first author Adalgisa Condoluci, MD, Department of Hematology, Institute of Oncology Research, Bellinzona, Switzerland, told Medscape Medical News
Continue reading this article on MedScape by registering for free
Patient With CLL May Have Had Longer COVID-19 Incubation Period
Patient With CLL May Have Had Longer COVID-19 Incubation Period
A case report out of China suggested that clinical and biochemical data of COVID-19 might have been partly masked in a patient with chronic lymphocytic leukemia (CLL).
Specifically, a patient presenting in Wenzhou, China, with CLL who was diagnosed with COVID-19 appeared to have a disease incubation period of about 25 days. The patient had traveled to Wuhan between January 12-18, 2020, before traveling back to Wenzhou and self-isolating for 14 days. He presented to the hospital on February 16 after four days of symptoms.
“Without the complete travel history, COVID-19 infection was not initially suspected, because his whole blood cell and lymphocyte counts were high because of his chronic lymphocytic leukemia masking a potential infection,” the case report authors wrote. “However, the attending physician noticed that although symptoms could be the result of a recurrent infection, his chest CT scan resembled that of a patient with COVID-19.”
After testing positive, the patient began treatment with reduced dose of oral chlorambucil to treat his condition due to CLL and received the recommended treatment for COVID-19 in China: nebulized α-interferon (5 million IUs) twice per day, intravenous human immunoglobulin (20 g) once per day, and intravenous methylprednisolone (40 mg) every 12 hours.
The patient had relapsing fever PaO2/FiO2 less than 300 mm Hg and a sequential organ failure assessment score of 4. Noninvasive ventilation therapy was given until dyspnea subsided on day 8 of treatment. Treatment was changed to low-dose methylprednisone every 12 hours with oral chlorambucil twice per day for the next 4 days.
Follow-up CT showed substantial improvement and the patient’s temperature also returned to normal. A repeat COVID-19 test showed the patient remained positive for the virus and an additional 7 days of observation was recommended.
Based on this case, the authors said better diagnostic strategies could be used for diagnosis, and individuals with compromised immune status may be subject to a longer disease incubation period.
“It remains uncertain whether the combination of chemotherapy, corticosteroids, α-interferon, and immunoglobulins could work synergistically in patients with chronic lymphocytic leukemia and COVID-19,” they wrote.
Coronavirus disease (COVID-19) and CLL patients
Coronavirus disease (COVID-19) and CLL patients
CLL Advocates Network is closely monitoring the strategies being implemented in various countries to manage the COVID-19 virus. Much of the information about COVID-19 does not address the concerns of people with chronic lymphocytic leukaemia (CLL). With this statement, we wish to fill this gap and provide extra advice for CLL patients.
The squeeze on healthcare in locked-down New Zealand
The squeeze on healthcare in locked-down New Zealand
Medical centres across the country are condensing services, moving online and ushering in pandemic plans. Josie Adams assesses what it’s like to access and provide essential medical care under alert level four.
On Monday, Sandra Russell woke up before dawn and drove to Milford to get her blood tested. She has an incurable blood cancer, myeloma, and needs weekly tests to see if the injections she gives herself are working to build her immune system. If she contracts Covid-19 now, it could kill her.
She has a poor immune system, so is used to self-isolating. “I’ve had two stem cell transplants, and you have to isolate yourself for six months afterwards,” she said. “I’m not going anywhere, but the one place I have to go is Labtests.”
Her usual centre is Devonport, but under alert level four she must go to Milford. She drove in the dark to join a line that was already growing. Inside the clinic, paper towels marked with Xs dotted every odd seat, so patients would maintain physical distance. When it was Russell’s turn, she was ecstatic to see her usually Devonport-based phlebotomist, who told her she’d had to buy her own face mask.
PPE not necessary
A release from Labtests last week stated that in order to protect the health of its phlebotomists, it would turn away patients with respiratory or feverish symptoms. When Russell attended the clinic on Monday, a young woman stood at the door screening patients with two questions: had they left the country in the past fortnight, and did they have any symptoms of Covid-19? She was employed by a security company, and was not medical staff. Russell saw her handed a jacket and t-shirt to wear during her shift, not a mask or gloves.
When approached, Labtests did not comment on specifics about its alert level four practices, but stated it had activated a pandemic plan that included limitations on the number of collection centres remaining open. In the statement, it said:
“There are a number of considerations with collection centre closures, including our ability to maintain safe staffing levels with the available personnel, our ability to operate in compliance with the requirements applicable during alert level four (such as physical distancing) and distribution of collection centres across the three Auckland DHB regions,” said a spokesperson. “The situation is developing rapidly and service levels are continually monitored.”
Labtests’ policies regarding personal protective equipment (PPE) are in line with current government guidelines.
According to the Labtests website, only 18 of its 60 Auckland clinics remain open. This is expected; many medical services are condensing or closing their services throughout lockdown, as only essential medical care will be provided face-to-face. For those with ongoing needs, blood testing will be available throughout alert level four. Home visits are only available to those with “urgent need“.
STIs going unchecked
Family Planning is one business that has turned off the lights in its premises nationwide.
Rose Stewart, national nurse advisor at Family Planning, said that although clinics are physically closed, staff are still working. Phone consults are available, and patients can book in for one via the website.
Stewart said many services were still accessible. “We can fax through prescriptions, and we can offer doctor’s consults,” she said. “You can still access abortions, too.” This was a major fear for many, but Stewart confirmed hospitals are still performing terminations where required and Family Planning is still providing information to patients.
One thing Family Planning is unable to do during alert level four is offer shots. “If you have gonorrhoea, we can’t treat you,” said Stewart. (In most cases, gonorrhoea is treated with a single injection of an antibiotic and a dose of tablets.) “But people probably aren’t spreading that right now.”
You might not know you have an STI; Labtests is focusing on Covid-19 samples, so if you’ve had a routine check for an STI recently it likely hasn’t been processed. However, if you have obvious symptoms you can still receive treatment. “We can treat chlamydia right now,” said Stewart. The symptoms are easily recognised and the treatment is antibiotics by prescription.
Those with IUDs, implants, and depo provera shots about to expire will also have to wait until the alert level decreases to get these updated by Family Planning. “If you are due for your depo provera jab or for your implant to be changed, we will give you a prescription for the pill until we’re able to do face-to-face appointments again,” said Stewart.
Jane Morgan of the Waikato Hospital Sexual Health Service said New Zealand was facing a syphilis epidemic when alert level four occurred, and medical services were still committed to treating STIs during this period. Syphilis is a destructive, eventually lethal infection, and its symptoms can take up to three months to show up. “Not everyone gets symptoms,” said Morgan. “We are still able to do syphilis blood tests for anyone with symptoms that suggest
Morgan said sexual health clinics and GPs would continue to offer services requiring face-to-face consults during this time, including gonorrhoea treatment and depo provera injections.
Not-so-general practice
The government has, more broadly, been directing healthcare providers to narrow their focus onto Covid-19. Three of Tāmaki Healthcare’s clinics — Airport Oaks, Henderson Specialist Centre, and St Lukes White Cross — are all now dedicated to testing for Covid-19.
FlexiHubs, discussed briefly in Friday’s press conference with director-general of health Dr Ashley Bloomfield, are being rolled out in greater numbers. These are clinics that will triage patients and test for Covid-19 away from the main medical centre, so patients with non-Covid-19 essential needs can be seen in relative safety.
Dr Alistair Sullivan, the director of Urgent Care Tāmaki Health, said that although they were redirecting resources to combating Covid-19, keeping things essential-only was affecting operation. “Attendance numbers are down by 50-60%,” he said. “We have consolidated our clinic operations by closing a small number of sites.”
The government has just announced $30 million in funding for GPs and pharmacies, to support management of the Covid-19 workload and community-based assessment centres. This came just as the Royal New Zealand College of General Practitioners announced GPs are a workforce in crisis.
“Financial assistance for general practice and urgent care clinics is necessary in order to protect the availability of primary health services now, and for the future,” said Sullivan. “Together we ensure that patients get the medical care they need close to their homes, and that our hospital system is free to deal with more serious medical presentations.”
Originally published on The Spinoff
How COVID-19 is Impacting Patients with Chronic Lymphocytic Leukemia
How COVID-19 is Impacting Patients with Chronic Lymphocytic Leukemia
As the new coronavirus (COVID-19) continues to spread around the world, concerns about how the virus impacts patients with cancer are mounting, making virtual connections between experts and patients a vital component of staying healthy.
To facilitate these connections, the CLL Society, a nonprofit organization focused on patient education, support and research, recently hosted part one of a virtual community meeting series where patients with chronic lymphocytic leukemia (CLL) spoke directly with experts about every aspect of the disease, from medication to clinical care and beyond, and how to get the best care possible during the pandemic.
Held via webinar on March 27, the meeting was designed to provide a link between patient questions and the CLL Society’s panel of experts, according to Patricia Koffman, co-founder and executive director of the organization. Dr. Brian Koffman, CLL Society co-founder, executive vice president and chief medical officer, who is also a 15-year CLL survivor, served as moderator, and was joined by a panel of experts from Lumere Healthcare Solutions, the University of Massachusetts, Memorial Sloan Kettering Cancer Center and Duke Cancer Institute.
Thomas E. Henry III, a clinical pharmacy advisor with Lumere and patient with CLL, kicked off the discussion with news about the CLL drug supply in the United States, as well as information on how patients can stay on top of their maintenance medication supply during the pandemic.
According to Henry, at the time of the presentation, the Federal Drug Administration reported no shortages for any commonly used CLL medications, including Imbruvica (ibrutinib), Calquence (acalabrutinib), Venclexta (venetoclax), Rituxan (rituximab) and others.
Although China is a major supplier of medications used in the US, the interruptions in production that occurred in certain regions due to the COVID-19 outbreak there did not impact US supplies and normal production is being resumed as the number of cases in China drop, Henry said. This has led to legislators considering new rules that would require more drugs to be made in the US.
As for how patients with CLL can ensure they don’t experience any gaps in dosage, Henry provided some strategies, including early refills and working with health care teams to modify dosages.
“A lot of people don’t know that your insurance will pay for a refill once you use 75% of the doses that were prescribed,” he said. “So, if you have ibrutinib, for example, and you have the 28-day supply, you can actually order that on the 21st or 22nd day and start to stockpile a little that way.”
This also applies to maintenance medications that help to mitigate CLL comorbidities. “Comorbidities increase the risk for patients that may contract COVID-19,” Henry explained.
“I think that patients need to be proactive and order their medications early. Don’t wait until you’ve taken your last pill to call the pharmacy.”
Susan J. Leclair, Chancellor Professor Emerita, University of Massachusetts and senior scientist with Forensic DNA Associates, LLC, then discussed the COVID-19 testing process and offered tips on how patients can modify their daily activities to stay safe from the virus.
“There’s a lot of stuff on the web right now about using various home chemicals to clean things,” said Leclair. “You can use alcohol, but you have to use alcohol that’s over 62%. So, unfortunately, unless you have a still in the backyard, and you can control this, using booze isn’t going to work. It’s too low.”
Dr. Anthony Mato, director of the CLL Program at Memorial Sloan Kettering Cancer Center, and Dr. Danielle M. Brander, associate professor of medicine at Duke Cancer Institute,
then fielded questions from the audience on topics like clinical trial participation and personal risk.
In the case of patients who are currently enrolled in clinical trials, Mato explained, participation should be continued wherever possible.
“Clinical trials are such an important part of the care of patients with CLL,” said Mato. “My stance has been that it is not in the best interest of patients to stop treatment in the context of a clinical trial, largely because we feel that the crisis with COVID-19 will pass and yet the CLL will still be present following that crisis, and so it is our duty to try and control the disease as best as possible.”
To reduce risk and exposure to COVID-19, Mato said, he and his colleagues work with patients on an individual basis to minimize the number of cancer center visits patients may need in the context of their trial. “We are largely switching to telemedicine visits, trying to do home labs and even shipping study drugs to patients. And we’re doing that on a large-scale basis within our CLL program,” he said.
Brander added that patients with CLL may be concerned about being at a higher risk of contracting COVID-19, and that she and her team are working with patients on an individual basis to help manage those concerns.
“The difficulty now, when you’re looking at (current COVID-19) studies, is bringing together a very diverse group of patients,” she said. “Their cancer might have been in a different location that kind of makes sense. (For example), lung cancer patients with active treatment, or recent surgeries are going to be very different maybe than patients with CLL. So, like Anthony (Mato) mentioned, this is why we’re trying to minimize your exposure with clinic visits.”
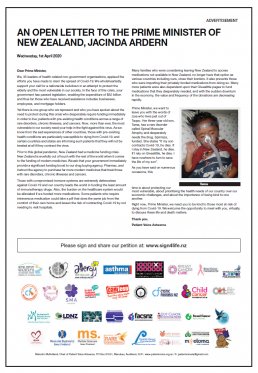
An open letter to the Prime Minister of New Zealand
An open letter to the Prime Minister of New Zealand, Jacinda Ardern
Urgently fund medicines to save the lives of our most vulnerable, defenceless citizens, ie those with pre-existing health conditions. That’s the message to the PM and her government in a full page ad in the Herald today organised by Malcolm Mulholland and the Patient Voice Aotearoa team, and supported by 35 patient advocacy groups. CLL Advocates are proud to be one of them and we congratulate and thank Malcolm and PVA’s generous supporters for this great initiative.
View the open letter by clicking the image below.
Covid 19 coronavirus: Pharmac eases restrictions on cancer drugs during Covid-19 pandemic
Covid 19 coronavirus: Pharmac eases restrictions on cancer drugs during Covid-19 pandemic
Pharmac will ease restrictions on at least nine cancer drugs, including keytruda for the treatment of advanced melanoma, to reduce hospital visits and cut the risk of highly vulnerable patients catching Covid-19.
One senior oncologist has praised the drug buying agency’s swift response, although patient advocates say cancer sufferers will need much more help during the pandemic.
Groups representing cancer patients are worried that the Givealittle pages many rely on to pay for medicines not funded by Pharmac won’t be supported in an economic downturn.
They also worry that if the health system becomes overloaded and ethical decisions have to be made about rationing ventilators then those with advanced cancer may not get access to them.
Some patients are already talking to their oncologists about whether they should pursue treatment at all – because some procedures, such as bone marrow transplants, heavily suppress the immune system and a Covid-19 infection may be a greater risk than stopping the treatment.
From this week Pharmac will make its first moves to help cancer patients in the pandemic by removing restrictions on keytruda, which is publicly funded for advanced melanoma, although not for lung cancer.
Oncologists will be able to give patients higher doses of keytruda, less frequently, in a bid to reduce hospital visits.
They will also ease testing requirements in order to free up access to at least eight other cancer drugs used to treat a range of conditions including prostate, breast and lung cancer.
Widening access for cancer drugs is part of a broader move by Pharmac to reduce the burden on the hospital system during the pandemic, although the agency will revert back to its previous rules once the crisis is over.
About 200 of the 2000 drugs publicly funded by Pharmac are subject to what is called Special Authority criteria, meaning patients require tests or consultations to get access to them.
Pharmac director of operations Lisa Williams said the agency was going through each of the 200 drugs which have Special Authority restrictions and waiving many of the barriers during the Covid-19 pandemic.
“The aim (is) to ensure that patients can still receive the medicines they need while we’re supporting the isolation principles as much as possible and freeing up resources in the health sector.”
Chris Jackson, a consultant medical oncologist at Dunedin Hospital, said Pharmac had been swift and agile responding to Covid-19, which poses a greater risk to the cancer patients he treats.
An analysis of Chinese data just published in The Lancet estimates people with cancer have 3.5 times the risk of suffering a severe Covid-19 infection.
“It’s really important to note that the health system at present is not overwhelmed in terms of its capacity and that means that all people who need cancer treatment will get their cancer treatment,” Jackson said.
But for those whose treatments heavily suppressed the immune system, such as bone marrow transplants, doctors would be talking to patients about whether that should go ahead given the risks of Covid-19.
“If we get to a level where we’ve got high rates of Covid infection in the community, we would seriously think very carefully about the balance of risks and benefits in individual patients,” Dr Jackson said.
“Because a lot of what we do, you can’t just turn off – it does take some time to wash out and as we have seen this epidemic can spread extraordinarily quickly.”
Another layer of risk was added for patients over 80. “If they get it and if you add a deeply immune-suppressing therapy to that then the balance of risks and benefits may tip against therapy. But that will be a discussion had with each individual patient.”
Malcolm Mulholland, spokesperson for Patient Voice Aotearoa, said there were a range of issues cancer patients were concerned about during the pandemic – including paying for drugs not funded by Pharmac.
Mulholland, whose wife Wiki Mullholland was diagnosed with Stage 4 breast cancer in 2018, said there were about 5000 Givealittle pages requesting money for medicines.
“It is, in effect, a de facto system being run because Pharmac is inadequately funded. That is a real fear amongst our community and quite simply, if these people don’t receive the medications they need, they will die.”
Philippa Reed, chief executive of Sweet Louise, which supports about 700 women with incurable breast cancer, said the charity had just launched an urgent appeal but fundraising was difficult during a lockdown.
“The kinds of community events that we may have had, have been cancelled. Any form of fundraising event, like most events, just isn’t happening.”
Reed also said members were worried after one was told by her oncologist that she may not get access to a ventilator in a situation where the health service became overwhelmed.
“Clearly New Zealand hasn’t got to that stage yet and so I think that was absolutely someone getting ahead of themselves. But with a particularly vulnerable community it’s really important not to drop your compassion and I think that was an example of just thoughtlessness.”
Jackson said patients with curable cancer who contracted Covid-19 should get the same care as anyone else.
Things may be different for those with advanced cancer who were approaching the end of their life.
“If you then get a Covid infection on top of that, which is severe and causing pneumonitis, it may well be that going on to a ventilator is an undignified death for those people.”
Jackson said ultimately patient rights and autonomy had to be respected.
“I’ve heard no conversations at all anywhere that said whole groups of people should not get ventilators. I have not heard anybody suggest that and I think anyone who made those broad brush types of statements would be seriously misguided.”
‘It is daunting to be told how personally dangerous coronavirus is’
‘It is daunting to be told how personally dangerous coronavirus is’
This story is behind a paywall, however if you have access or sign up for a free trial you’ll be able to read the full article by Sam O’Neill, a UK reporter with CLL. Access the full article here: https://www.thetimes.co.uk/article/coronavirus-it-is-daunting-to-be-told-how-personally-dangerous-this-virus-is-7qbfqxl9k
I have never before considered myself to be a vulnerable person. As a reporter, much of my work has been about highlighting the plight of the vulnerable.
Today, however, I expect a letter from the NHS telling me that I am “extremely vulnerable” if I contract Covid-19. It will tell me to stay at home for at least 12 weeks and will be followed periodically with text messages giving advice and information. I am part of the group with what are so often blandly referred to as “underlying health conditions”. My problem is chronic lymphocytic leukaemia (CLL), which means my body makes too many white blood cells. Left unchecked these will crowd out the red cells and threaten vital organs.