‘It is daunting to be told how personally dangerous coronavirus is’
‘It is daunting to be told how personally dangerous coronavirus is’
This story is behind a paywall, however if you have access or sign up for a free trial you’ll be able to read the full article by Sam O’Neill, a UK reporter with CLL. Access the full article here: https://www.thetimes.co.uk/article/coronavirus-it-is-daunting-to-be-told-how-personally-dangerous-this-virus-is-7qbfqxl9k
I have never before considered myself to be a vulnerable person. As a reporter, much of my work has been about highlighting the plight of the vulnerable.
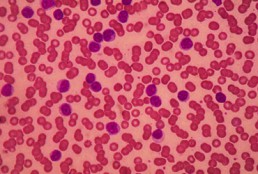
Today, however, I expect a letter from the NHS telling me that I am “extremely vulnerable” if I contract Covid-19. It will tell me to stay at home for at least 12 weeks and will be followed periodically with text messages giving advice and information. I am part of the group with what are so often blandly referred to as “underlying health conditions”. My problem is chronic lymphocytic leukaemia (CLL), which means my body makes too many white blood cells. Left unchecked these will crowd out the red cells and threaten vital organs.
Coronavirus: how Asian countries acted while the west dithered
Coronavirus: how Asian countries acted while the west dithered
The first coronavirus cases in Taiwan and Italy came only 10 days apart. On Sunday Taiwan, which has deep cultural and economic ties to China, has recorded just 153 cases and two deaths. Italy has more than 47,000 cases and 4,032 people have died.
Italy’s epidemic is currently the most devastating in the world; its death toll overtook China’s last week and on Saturday officials in Lombardy said deaths in that region had jumped by 546 in one day to 3,095. The pattern of an exponential explosion in cases, after weeks of government inaction in the face of impending crisis, has been repeated across western countries from Spain, France and Germany, to the UK and the US.
Leaders are now taking measures that would have been unthinkable weeks or even days ago, locking down tens of millions of people from Berlin to Madrid and San Francisco and pouring billions into rescue plans.
But had they acted a few weeks earlier, they could perhaps have avoided much of the human tragedy and economic catastrophe they now face. Taiwan, Hong Kong and Singapore, which had their first confirmed cases before Europe, but acted early and fast, still have deaths in single digits and, at most, a few hundred cases.
Taiwan, helped perhaps by having an epidemiologist as vice-president, started tracing passengers from Wuhan as soon as China warned of a new type of pneumonia in the city last December, before Covid-19 was identified. Social distancing, ramped-up testing and contact-tracing followed soon after.
Most western countries did little, apart from developing a modest testing capacity – apparently gambling on the disease being contained elsewhere, as previous threatened epidemics, including Sars in 2002-03 and more recently Ebola and Mers, had been.
“The challenge faced by government is whether and when to act on a health threat. If you act swiftly and the outbreak isn’t as bad as feared, then government gets criticised for overreacting. If you adopt a wait-and-see approach and move too slowly, then government gets criticised for underreacting,” says Steve Taylor, professor at the University of British Columbia and author of The Psychology of Pandemics.
“In hindsight, the UK might have been better off if they had adopted the same practices as Taiwan. But if the outbreak had fizzled, the government would have been criticised for overreacting. Taiwan gambled successfully on the assumption that Covid-19 would spread widely and rapidly.”
Other countries that initially allowed the disease to spread – most notably South Korea, which at one point was the country with the most infections outside China – managed to partially tame the outbreak through rigorous testing and tracing contacts of those infected. Subsequently, new infections levelled off, even as they spiralled across Europe.
“I do think we can learn from past mistakes, and South Korea is a really strong example of that if you look at the amount of testing they have been doing, and how fast they were able to mobilise,” said Ashley Arabasadi, chair emeritus of the Global Health Security Agenda Consortium.
“It might be unfair to criticise governments that haven’t had to deal with something like this in over 100 years, while South Korea have had more recent experience.”
South Korea’s sense of urgency was driven in part by recent firsthand experience of how virulent coronaviruses can be due to an outbreak of Mers in 2015 and the 2002-03 Sars epidemic, which also affected Taiwan, Hong Kong and others in the region.
Those diseases barely touched the west, being contained, like others including Ebola, near the site of their outbreak, potentially leaving the west’s leaders too complacent.
“We should have used that time [in January and February] more wisely, but, to be fair, everyone was dealing with an unknown,” said Laura Spinney, a science journalist whose latest book is Pale Rider: The Spanish Flu of 1918 and How it Changed the World. Authorities didn’t want to cause panic initially, she said, but then the balance shifted so “the biggest danger was not panic – it was complacency, and too many governments weren’t moving”.
There is a chance some politicians in the US and Europe, lulled by decades of stability in their countries after the second world war – decades in which they have waged war overseas but never seen life totally upended at home – simply didn’t want to recognise the threat.
“People are not terribly good at estimating risk. Wishful thinking, overestimation of resources, and other factors can cloud our judgment of risk. This may have happened during the current pandemic,” Taylor said.
It’s important, however, that whenever the world does successfully develop a vaccine, or a cure for Covid-19, the tragic lessons of these early crises are not forgotten. Governments need to invest in healthcare systems, so that when the next pandemic arrives, we are better prepared.
“You see a system of panic and response that we go into. Once that initial panic dies down, you get complacency, a lack of understanding that these novel viruses happen regularly and will happen with greater frequency as we become more interconnected,” said Arabasadi. “That’s why there needs to be a greater investment in health and health systems.”
Originally published on The Guardian
Coronavirus in NZ: How to self-isolate - Kiwi diagnosed with cancer shares advice
Coronavirus in NZ: How to self-isolate - Kiwi diagnosed with cancer shares advice
A Kiwi diagnosed with cancer has shared advice on how to self-isolate while living with others and what precautions immunocompromised people should take.
The Government has announced that people travelling into New Zealand, except from the Pacific Islands, have to self-isolate for 14 days.
This has sparked many questions on how self-isolation works and how to deal with it when more than one person lives in a home.
Auckland man, Earle Wilco, 44, moved to Island Bay, Wellington, from Shanghai when he was diagnosed with chronic lymphocytic leukaemia (CLL) last December.
“Mid-cycle, my immune system drops and I become very susceptible to infections, colds and flu,” he said.
He has had to self-isolate during these times while living with his friend and his two children, aged 11 and 14.
After seeing a friend in Wellington seeking advice on how self-isolation works, Wilco has shared his knowledge through his own experiences, which also includes self-isolation during a norovirus outbreak in 2005.
“Self-isolating in a house share is particularly tricky, but it can be done if all the housemates pull together,” he said.
“My suggestion for someone returning from overseas who has to self-isolate in a house share situation is this:
“1. Inform everyone of your arrival time so they can clean the house. Make it clear that you’ll need help with food shopping and even cooking sometimes, set up bank transfers with all housemates so you can pay them if you ask them to buy you stuff. Set up a special house WhatsApp group chat.
“2. Once home, stay in your room as much as possible. If there’s more than one bathroom in the house, have one dedicated only to you, this will remove a lot of cross-contamination potential. Likewise, keep your own sheets, towels and cutlery separately. (If you can’t have a dedicated bathroom, make sure you wipe down all surfaces with disinfectant after you use it).
“3. If you have to be out of your room when others are around, wear a mask, wash your hands, and wipe down surfaces that you touch.
“4. Food can be delivered to your bedroom door. They knock, walk away, you retrieve it.
“5. Make sure you have a digital thermometer, and check your temperature regularly. If it gets above 37.5, call your GP or after-hours clinic, outline your situation and wait for advice.”
Wilco’s advice is very similar to the advice given by the Ministry of Health and other disease experts including University of Otago epidemiologist Professor Michael Baker.
“It’s not home detention – people can wander around the streets and get some exercise. The thing is about not infecting other people if you might be in the early stages of incubating this infection,” Baker previously told the Herald.
During his chemo self-isolation periods, Wilco said he follows all these guidelines along with more.
“I try to time cooking and using shared spaces when everyone is out,” he said.
“This is as much for my safety as the safety of my housemates, as when you’re doing chemo, you’re awash with toxic chemicals which come out in your body waste.”
Wilco said the precautions he is taking now because of the Covid-19 outbreak are the same as he uses when his immune system is low.
This includes limiting travel, staying away from groups of people, sticking to his room whenever possible, eating healthy, washing hands frequently and keeping his distance with others.
Meanwhile, Wilco said he hasn’t had any problem with Covid-19 as he left China before the outbreak. However, his wife is stuck in China.
“She went back to Anhui Province for Chinese New Year and got caught there with the city lockdowns, so she was in quarantine for about 50 days, only allowed to leave the house once a day for supplies,” he said.
“She has just got back to Shanghai last week and has to self-isolate for another 14 days.
“We also have a lot of friends in Wuhan, so we get lots of information and advice. The stories are frankly heartbreaking.”
His last piece of advice was for people not to panic.
“It is a pandemic and it is taking lives, it needs to be taken seriously, so the best thing people can do is limit close personal interactions and practice good hygiene.”
Immunocompromised precautions
According to the Ministry of Health, those who are underlying medical conditions, such as a compromised immune system, liver disease, cancer, kidney disease, heart disease and diabetes mellitus, need to take more precautions to protect themselves from Covid-19.
It recommends immunocompromised people to take the following simple steps to protect yourself and others:
• Avoid close contact with people with cold or flu-like illnesses.
• Cover coughs and sneezes with disposable tissues or clothing.
• Wash hands for at least 20 seconds with water and soap and dry them thoroughly:
– before eating or handling food
– after using the toilet
– after coughing, sneezing, blowing your nose or wiping children’s noses
– after caring for sick people.
There are also additional measures that immunocompromised people should take:
• Avoid staying with a person who is self-isolating (because they are a close contact of a confirmed case of Covid-19 or have recently travelled to any country except those listed in the countries and areas of concern under Category 2.)
• Stay at least 2 metres away from people who are unwell.
• Checking safe travel advice about Covid-19 if you plan overseas travel.
• Those who take immunosuppressive drugs we advise that you do not stop this medication without first consulting your GP or specialist.
Originally published on the New Zealand Herald
Coronavirus: how to self-isolate
Coronavirus: how to self-isolate
What to do if you have symptoms of Covid-19, have travelled to a badly affected area, or have been in contact with someone who has the disease.
1. Stay at home
This may sound obvious, but don’t leave home except to get medical care (and if you do, make sure you have called ahead). Say no to visitors. Contact friends and family online or by phone. If you use online shopping for deliveries of food, medicine or other necessities, make sure delivery instructions say that items should be left outside, not handed over in person. If you ask friends or family for help bringing you supplies, get them to do the same.
2. Separate yourself from others
Stay in one room, with the door closed – ideally a room that has a window to the outside that you can open. Don’t share crockery, cutlery, glasses, bedding or towels with anyone in your home when you have used them. Dishwashers can be used to clean crockery and cutlery. If that isn’t possible, wash by hand and dry using a separate tea towel. Laundry, bedding and towels should be placed in a plastic bag and washed only when tests for Covid-19 are negative or self-isolation is over, if possible. Do not take anything to a launderette. If you have to wash at home, use temperatures of at least 60C.
3. Food and bathrooms
Have meals left outside your door. If you cook for yourself, do so, if possible, when others are not in the kitchen – and take food back to your room to eat. If you have more than one bathroom in your home, use a separate one. If you have to share, ensure you clean it thoroughly and regularly. If you live in shared accommodation (such as university halls of residence), leave your room only when necessary, ideally wearing a mask, if you have one. Try to avoid using the kitchen or bathroom while others are there.
4. Keep away from pets if possible
Wash your hands before and after contact as a precautionary measure.
5. Safely dispose of tissues after you cough or sneeze
Dispose of them into a plastic bag and immediately wash your hands with soap and water, and dry thoroughly. If you have one, wear a mask when you are in the same room as others, or if you go out for medical treatment.
6. Hand washing
The rules are similar to those for all people – wash your hands often and thoroughly, using soap and water, for 20 seconds Then rinse and dry thoroughly. Avoid touching your eyes, nose and mouth with unwashed hands.
7. Waste disposal
All waste that you have been in contact with, including used tissues and masks, should be put in a plastic rubbish bag and tied when full. The plastic bag should then be placed in a second bin bag and tied. Do not dispose of it or put it out for collection until you have test results, or until quarantine is over. If you test positive, you will get instructions on how to dispose of the waste.
8. If symptoms worsen
Seek medical help quickly if you develop new symptoms or if your symptoms worsen (for example, if you have problems breathing).
COVID-19 and CLL
COVID-19 and CLL
This article was originally published on CLL Society
We are receiving many requests to suggest any special precautions for us, CLL patients, in response to the spreading risk of coronavirus (COVID-19).
First, this is an evolving situation with more unknowns than knowns at the present time.
Second, it does appear that those over 60 years old are at increased risk for a more serious infection. That would include many of us CLL-ers.
Next, those who are immune suppressed (and all CLL patients, whether treated or not, are immune suppressed) are at a higher risk for serious disease, but perhaps there is less of an increased risk for us than for those with heart or lung conditions. There is almost no data out there to provide clarity on this important issue.
There is also no clarity as to whether we are at higher risk to acquire the infection, only that we are more likely to have a rough time if we do get it. So far it does not appear that we are at higher risk to become infected, but again there is just too little information to be certain at this time.
The prudent course of action is to follow the CDC and WHO guidelines that, besides hand washing, elbow bumps, avoid touching your eyes, nose, and mouth, cleaning and disinfecting frequently touched objects and surfaces, and more, now the CDC advises high risk folks like us to avoid travel and crowds. This was a change as of March 5, 2020.
In a proactive and cautionary move, the CLL Society canceled all Support Group meetings and Patient Educational Forums scheduled for March. Soon after announcing this, LLS and LRF canceled meetings as well.
For general information from the CDC, please see: https://www.cdc.gov/coronavirus/2019-ncov/about/index.html and for high-risk populations, including CLL patients, see: https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.htmlI myself have canceled 2 trips for CLL-related education this month.
The CLL Society is closely monitoring the COVID-19 outbreak and will provide updates through the website, and will, when appropriate, through our email list, as soon as more information becomes available. Rather than sending individual emails with your questions, please sign up for our Alerts and check the website for the latest COVID-19 news.
30 tips for living well with CLL (an update of "Coping Strategies" and "Things we can do...")
30 tips for living well with CLL (an update of "Coping Strategies" and "Things we can do...")
This is a collection of practical tips gathered from this forum over the years, to help us live better with CLL. I’ve added some personal comments, saying how I myself have taken on board some of these suggestions.
Single-cell sequencing of CLL therapy: Shared genetic program, patient-specific execution
Single-cell sequencing of CLL therapy: Shared genetic program, patient-specific execution
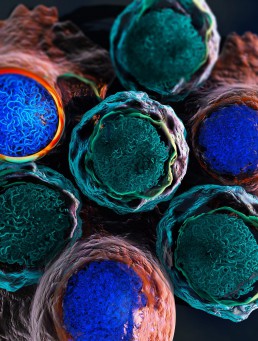
Chronic lymphocytic leukemia (CLL) is the most common form of blood cancer (leukemia) in the Western world, affecting approximately 1.2% of all cancer patients. This type of cancer starts with the lymphocytes (a type of white blood cells) that are produced in the bone marrow. CLL is characterized by the proliferation of abnormal lymphocytes (B cells) that fail to mature and grow out of control. These abnormal cells accumulate in the bone marrow and lymph nodes, taking the place of other healthy cell types and impeding their normal development. Finding the most suitable therapy for each patient poses a challenge due to the clinical and molecular heterogeneity of this disease, with some patients facing slow disease progression, whereas others face rapid progression and require quick medical response.
The cancer drug ibrutinib, a Bruton tyrosine kinase (BTK) inhibitor, has remarkable efficacy in most patients with CLL. It is becoming the standard of care for most patients requiring treatment due to its clinical efficacy and mostly tolerable side effects. However, it does not cure the disease, and patients must undergo prolonged periods of treatment. Christoph Bock and his group at CeMM investigated the molecular program with which CLL cells and other immune cells response to ibrutinib treatment in patients with CLL. Their goal was to learn the epigenetic and transcriptional patterns that predict how swiftly the treatment is having an effect on the CLL cells and how long it takes for the disease to respond in each individual patient.
More Specific BTK Inhibitor Shows High Relative Rates of Response in CLL
More Specific BTK Inhibitor Shows High Relative Rates of Response in CLL
In a phase 3 trial, acalabrutinib, a second-generation Bruton’s tyrosine kinase (BTK), provided a progression-free survival (PFS) advantage over a chemotherapy-containing standard in frontline treatment of chronic lymphocytic leukemia (CLL).
In the three-arm study, called ELEVATE TN, acalabrutinib (Calquence, AstraZeneca) alone and in combination with obinutuzumab (Gazyva, Genentech) was found to be significantly more effective than chlorambucil plus obinutuzumab for the primary PFS end point, reported investigator Jeff P. Sharman, MD, at the 2019 annual meeting of the American Society of Hematology (ASH, abstract 31). Dr. Sharman, the director of research at Willamette Valley Cancer Institute, in Eugene, Ore also noted that a trend toward an overall survival (OS) benefit appeared to be emerging for the acalabrutinib combination.
Slides from Edinburgh
Slides form Edinburgh
Why are Online Communities a Good Idea?
- A new diagnosis can be a scary, and lonely, time.
- Online communities like CLLANZ, HealthUnlocked, and Patient Power are helping people come together, and cope with complex chronic illnesses such as CLL.
- The patients’ shared experiences and knowledge of their condition, hospitals, healthcare services and drugs is leading to improvements in patient care, both by themselves, and by their carers, and their doctors.
- Knowledgeable patients become their own advocates and ask questions of their doctor, forming a partnership approach.
Chronic Lymphocytic Leukaemia
- Most common adult leukaemia
- Most patients are older than 65
- Cancer of the immune system affecting B-cells
- Can present with a weak immune system
- Each patient’s CLL is different
- Most patients will, often initially, not require treatment. Watch and wait (and worry)
- Most new therapies have improved the prognosis of CLL, but it still remains a chronic condition that can only rarely be cured
Initial Workup of CLL Patients
- All patients at diagnosis
-Flow cytometry (via blood and / or bone marrow) to confirm CLL diagnosis
- Informative for prognosis and / or therapy determination
-Del17p, and del11q. These portend for more aggressive disease
-Mutated / unmutated VH gene status assessment (not yet available in New Zealand).
-No CT scan unless symptoms are present: PET scan can be helpful if Richter’s suspected
- Bone marrow biopsy and aspirate not necessary in absence of cytopenias
Ibrutinib and Venetoclax Combo ‘Impressive’ in Front-Line CLL
Ibrutinib and Venetoclax Combo ‘Impressive’ in Front-Line CLL
The combination of two targeted therapies — ibrutinib (Imbruvika, Pharmacyclics/Janssen) and venetoclax (Venclexta, AbbVie) – has shown impressive results in the front-line treatment of chronic lymphocytic leukemia (CLL).
To read the full story visit Medscape