Higher Overall Response Rates Observed When Adding Ublituximab to Ibrutinib Treatment for CLL
Higher Overall Response Rates Observed When Adding Ublituximab to Ibrutinib Treatment for CLL
This article was originally published on CancerNetwork
The combination of ublituximab plus ibrutinib (Imbruvica) led to a statistically higher overall response rate while maintaining the tolerable safety profile over ibrutinib monotherapy to treat patients with relapsed or refractory high-risk chronic lymphocytic leukemia (CLL).
According to data published in The Lancet Haematology from the phase 3, multicenter, GENUINE (NCT02301156) trial, these findings support the addition of ublituximab to Bruton tyrosine kinase (BTK) inhibitors as treatment for patients with this class of CLL.
“Clinically meaningful improvements in overall response rate, complete response, and MRD negative response were observed and translated into improved progressionfree survival,” wrote the investigators. “These findings indicate the benefit of adding the nextgeneration antiCD20 antibody ublituximab to ibrutinib in patients with relapsed and refractory high-risk chronic lymphocytic leukaemia.”
The overall response rate was 83% of patients in the ublituximab plus ibrutinib group and 65% of patients in the ibrutinib group (P = .020) after a median follow-up of 41.6 months (IQR 36.7–47.3).
While the safety profile consisted mostly of grade 1 or 2 adverse events, neutropenia (19% of patients in the combination group vs 12% in the control group), anemia (8% vs 9%, respectively), and diarrhea (10% vs 5%) were common grade 3 and 4 adverse events among the population of interest.
More, common serious adverse events included pneumonia (10% with ublituximab vs 7% with ibrutinib only), atrial fibrillation (7% vs 2%, respectively), sepsis (7% vs 2%), and febrile neutropenia (5% vs 2%).
Two patients from the ublituximab plus ibrutinib group and 5 patients and from the ibrutinib group died from adverse events. Only 1 death (cardiac arrest) from the ibrutinib group was considered treatment-related.
Webinar: The current CLL treatment landscape and advocating for your care
The Current CLL Treatment Landscape and Advocating for Your Care
Overview
Join us for a virtual town hall meeting for chronic lymphocytic leukemia (CLL) patients and family members on Saturday, March 20, 2021 starting at 10 am CT/11 am ET. – 5am, Sunday 11 March NZST
This 3-hour program will take you through the current treatment landscape of CLL, including the latest news in research, state-of-the-art testing and personalized care. Our speakers will offer advice on advocating for the best of care, staying informed and playing an active role in your treatment journey. Join our hosts Carol Preston, Andrew Schorr and Michele Nadeem-Baker for this informative session on living with CLL. Our special guests include Shuo Ma, MD, PhD, and Nurse Practitioner Jennifer Boyer, MSN APRN NP-C, of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, as well as Deborah M. Stephens, DO, of the Huntsman Cancer Institute at University of Utah and Jane Dabney, LISW-S, OSW-C, Senior Oncology Social Worker at Cleveland Clinic.
Agenda
10:00-10:30 am CT – Introduction: Information for those who are newly diagnosed or beginning their treatment journey. Learn about the stages of CLL and questions to ask your doctor.
10:30-10:45 am CT – CLL and COVID-19: What should patients know about the COVID vaccine? Is it safe to start or resume treatment right now? Get the latest updates on COVID-19.
10:45-11:30 am CT – The Treatment Landscape: Learn about the current CLL treatment landscape, including the latest news in research, state-of-the-art testing and options for personalized care.
11:30-11:45 am CT – Break
11:45-12:30 pm CT – Being Your Own Advocate: Experts and patient guests discuss how patients and care partners can advocate for the best of care, stay informed, and play a more active role in their treatment.
12:30-1:00 pm CT – Q&A
Send us your questions: cll@patientpower.info
Learn more here and register to attend
CLL Can Leave You Immunocompromised. Here’s How to Manage
CLL Can Leave You Immunocompromised. Here’s How to Manage
This article was originally posted by Healthline
- Chronic lymphocytic leukemia (CLL) is a type of cancer that attacks white blood cells, affecting your body’s ability to fight off infection.
- CLL leaves you immunocompromised, increasing your risk of infection, other cancers, autoimmune conditions, and severe complications from COVID-19.
- Taking steps to stay healthy and boost immunity can help you stay well with CLL.
Your bone marrow plays an important role in your body. It produces versatile stem cells that become specific types of blood cells. Red blood cells transport oxygen to the body, platelets stop bleeding, and white blood cells combat infection to keep you healthy.
Chronic lymphocytic leukemia (CLL) is a type of cancer that starts in your bone marrow. CLL changes your infection-fighting white blood cells and interferes with how they function. As a result, CLL weakens the immune system.
Read on for more information, plus tips for how to manage being immunocompromised when you have CLL.
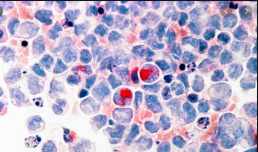
There are several types of white blood cells, but lymphocytes are the ones primarily involved in CLL.
Healthy lymphocytes protect you against viral, bacterial, and fungal infections that can make you sick. When you have CLL, your body produces abnormal lymphocytes called leukemia cells, which don’t fight infection as well as lymphocytes.
With CLL, your bone marrow still produces normal white blood cells, but the leukemia cells multiply faster and live longer than the healthy ones. As they reproduce, these leukemia cells take over space in your bone marrow, leaving less room for healthy white blood cells. Because the leukemia cells don’t fight infection well, as their numbers increase, your immunity decreases.
The epic battle with cancer's 'Death Star'
The epic battle with cancer's 'Death Star'
This article was originally posted by The Guardian.com
In the early 1980s, Channing Der was just beginning his career as a scientist at Harvard Medical School when he happened upon a discovery that would change the course of cancer research. At the time, the holy grail of cancer biology was discovering so-called oncogenes – genetic switches that can turn a normal cell into a cancer cell – in the genomes of tumours. But while teams of scientists had thrown everything at it for the best part of a decade, their efforts had proved fruitless. One by one, they were beginning to accept that it might be a dead end.
Der found himself assigned to test 20 different genes that had been identified as possible oncogene candidates. His question was simple: did any of them actually exist in tumours in a form that was different from normal cells?
“People thought it wasn’t going to work,” he remembers. “I began, and certainly for five months, the chances of success seemed to be pretty slim. I was ready to just wrap this up, and move on to something else that might be more productive, when I made the discovery which changed the course of my professional career.”
The first 18 of the genes Der tested turned out to be normal. But the final two, members of a gene family called RAS, were found to be uniquely mutated in cancer cells. “Being fairly new to the field at that point, I didn’t fully understand the ramifications of what this meant,” he laughs. “I was working in the lab of a professor named Geoffrey Cooper, and when I showed him the results, he paused for what seemed like minutes. So I asked if he was OK, and he replied: ‘This could be one of the most significant discoveries in cancer biology in decades.’”
R. Gregory BD, discusses outcomes for patients with chronic lymphocytic leukemia and COVID-19.
R. Gregory Bociek, MD, discusses outcomes for patients with chronic lymphocytic leukemia and COVID-19.
This article was originally posted by Onclive
R. Gregory Bociek, MD, an associate professor of internal medicine, Division of Oncology and Hematology and program director, Hematology/Oncology Fellowship Program, University of Nebraska Medical Center, discusses outcomes for patients with chronic lymphocytic leukemia (CLL) and COVID-19.
One retrospective, multi-institutional study included 198 patients with COVID-19 and CLL across 43 institutions, according to Bociek. Data showed that approximately one-third of patients will not survive; the overall case fatality rate was 33%, Bociek says. Additionally, one-third of patients were intubated, or admitted to the intensive care unit, and 90% of patients were hospitalized.
Despite the fact that the investigators have done their best to collect data, they’re more likely to think of patients who are sicker, according to Bociek. Additionally, the first few papers to be released could make the situation seem more dire than it actually is, Bociek adds. However, several lessons can still be taken away from the paper, such as that patients with more comorbidities and organ dysfunction may represent more challenging cases, Bociek concludes.
CLL Advocates Newsletter Issue 8
CLL Advocates Newsletter Issue 8
Dear Friends of CLLANZ
New Zealand’s Covid 19 national vaccination programme kicked off last week.
For people with CLL, Covid 19 has additional risks above those of the general population.
There is an increased risk of infection, and, in particular, an increased mortality for CLL patients who get severe disease. Some of this relates to the age group typically affected by CLL, and some to the intrinsic immunodeficiency that is part of CLL.
In a recent study from the European Research Initiative on CLL (ERIC), about 80% of patients in a study on Covid 19 in CLL patients had severe disease. Over a third of these patients died of Covid 19 infection. Being on ibrutinib seemed to have a protective effect, reducing the severity of the disease.
Vaccination immune responses are reduced in people with CLL, so vaccination likely will not provide as good a level of protection in this group as in the general population.
There is much that has been found so far from vaccination programmes in other countries, and from the research that has been done, and that continues to be done.
There are many vaccines in development for Covid 19, and three of those have been approved for public vaccination programmes.
There are the mRNA vaccines of Pfizer/BioNTech, and Moderna; and the AstraZenica/Oxford vaccine that uses a chimpanzee cold virus as a vector. The latter, I am told, is considered safe to use in CLL patients by most UK haematologists.
Some other information to look out for:
- Studies are in progress regarding using more than one vaccine in the same individual.
- There was a study that used half the recommended dose for the initial vaccine and then a full dose for the second, which seemed to have been associated with a better outcome than the orthodox vaccine recommendation.
- The interval between vaccine doses when the vaccine is orthodoxly given in two doses is the source of some debate, and a longer interval seems OK.
- Response rates for vaccines in use has been high, with some variation in subgroups, but the duration of vaccine protection seems to be variable, and still being studied.
So, vaccination is recommended for people with CLL, and you should seek medical advice regarding getting your “jab”
Best wishes
Neil Graham
Limited Following of Best Practices for CLL Observed in the Real-World Setting
Limited Following of Best Practices for CLL Observed in the Real-World Setting
Anthony Mato, MD, MSCE, a hematologic oncologist and director of the CLL Program at Memorial Sloan Kettering Cancer Center, discusses an observational registry study of real-world prognostic biomarker testing, treatment patterns, and treatment dosing in a pool of 1461 patients with either chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia.
The uniqueness of performing a registry study is that it provides the opportunity to see if oncology practices are following the recommendations of governing bodies like the National Comprehensive Cancer Network, and the International Workshop on CLL, says Mato. Also, with a large collection of new data being released at medical conferences each year, prospectively evaluating the field can show how the latest treatment strategies are being implemented.
Results from the study were eye-opening, Mato explains. It was shown that a small proportion of patients treated in the real-world had the recommended prognostic biomarker testing. Because of this lack of testing, oncologists made treatment decisions that would not be considered the standard in today’s treatment landscape. Instead of administering ibrutinib (Imbruvica) or another targeted therapy to patients with del(17p) or TP53-mutated disease, the data showed that oncologists gave chemoimmunotherapy, Mato notes.
Supplements, My Treatment Approach: Chronic Lymphocytic Leukemia, Volume 1, Issue 1
Supplements, My Treatment Approach: Chronic Lymphocytic Leukemia, Volume 1, Issue 1
This article was originally published on OncLive
The addition of BTK inhibitors to the treatment arsenal for patients with chronic lymphocytic leukemia (CLL) has resulted in improved survival and quality-of-life (QoL) outcomes, according to Tara Graff, DO, and the next steps for research is to examine these agents head-to-head, as well as in doublet and triplet regimens, in the hopes of providing added benefit.
“This is an exciting time for the field of CLL. Among the many hematologic malignancies, CLL seems to be on the frontline now, especially in terms of the different therapies [available] and research [that is being done],” Graff said. “We’re offering our patients better treatments that are allowing them to live longer, with a better quality of life [QoL]. This is very important. We are talking about a chronic disease that is not curable, so the fact that we’re able to help patients maintain their QoL is astonishing.”
The emergence of the BTK inhibitors ibrutinib (Imbruvica), acalabrutinib (Calquence), and zanubrutinib (Brukinsa) into the treatment paradigm improved outcomes for patients with this disease. To build on that benefit, investigators are now investigating these agents in novel combination regimens. Triplet approaches are an important area of interest, according to Graff.
For example, the time-limited combination of ibrutinib, venetoclax (Venclexta), and obinutuzumab (Gazyva) was found to elicit an overall response rate of 84% in treatment-naïve patients with CLL and 88% in those with relapsed/refractory disease.1 Moreover, the acalabrutinib is also under investigation in combination with venetoclax and obinutuzumab or rituximab (Rituxan). Results have shown that that acalabrutinib in combination with a CD20 antibody and a BCL-2 inhibitor resulted in an ORR of 92% in those with relapsed/refractory disease; notably, the ORR was even higher in those who were treatment naïve, at 100%.2
CLL Advocates Newsletter Issue 7
CLL Advocates Newsletter Issue 7
Dear Friends of CLLANZ
Happy New Year to you all out there in CLL land.
Last year has been an extraordinary one for humanity and the planet.
But perhaps better news for CLL and other blood cancers for the year to come, from the other side of the ditch (the Western Isle), and the potential to develop a similar initiative in Aotearoa. Over the last four years, Leukaemia Foundation Australia has developed a bold project, with the expressed ultimate aim being zero lives lost to blood cancers by 2035.
In the four years to 2020, much good work has been done by many to create the recently launched Australian National Action Plan for Blood Cancers. Details are available in the document of the same name, released in June 2020. The main themes are: best practice clinically, empowerment of patients and their families, accelerated research, and access.
There has also been an interesting article in the most recent Patient Power about diet and CLL, which you should all find interesting. This one is on diet and supplements, and this one on how diet can prolong the ‘watch and wait’ period.
Best wishes
Neil Graham
For Younger Patients, CAR T-Cell Therapy Could Play a Role in CLL Treatment
For Younger Patients, CAR T-Cell Therapy Could Play a Role in CLL Treatment
This article was originally published on Cure
In an interview, Dr. Matthew Davids of the Dana-Farber Cancer Institute discusses the future of CAR T-Cell therapy in the treatment of younger patients with chronic lymphocytic leukemia.
While there are risks involved with CAR T-cell therapy, it could become a more popular therapy choice for younger patients with chronic lymphocytic leukemia (CLL) compared to bone marrow transplant, which can be even more difficult to tolerate, says Dr. Matthew Davids of the Dana-Farber Cancer Institute.
In an interview with CURE®, Davids explained that younger patients with CLL, particularly those with more high-risk disease who have relapsed despite a number of previous treatments, could find CAR T-cell therapy treatment a more tolerable option than the standard of allogeneic transplantation.
By harnessing and reprogramming the body’s own cells to fight cancer, CAR T-cell therapy has had success in a number of other cancer types in the past decade or so, Davids noted. And while it’s not currently approved for use in CLL, it is being examined in various combinations that could prove successful down the road.
Transcription:
One other thing that comes to mind as we think about where the field is headed in the future is that we’ve seen some early but promising data for CAR T-cell based therapies. This is using the patient’s own T lymphocyte cells, educating them outside the body and then reinfusing them to try to have a sustained response to CLL.
And although this is not yet an FDA approved treatment in CLL, I think it’s showing promise. I think about it for my younger patients, particularly those who have maybe been through a few lines of CLL treatment already, particularly if they have very high-risk disease like the TP53 deletion or mutation. You know, currently, those are patients we think about bone marrow transplant, allogeneic transplantation for, but that certainly has some very serious risks. And even though CAR T-cell therapy also has risks, I think, in general, the toxicity profile is more favorable than allogeneic transplantation.
We’ve started to see some patients with very long-term remissions now from CAR T. So I’m excited to see the how that field evolves in the coming years. There are people exploring various combinations of different drugs with CAR T. And so, I think the technology and the combination therapies will improve over time. And so I do think that for younger patients who have a long time horizon, that could eventually be an approved option to think about down the road.