Experts Discuss Treatment Advances for Chronic Lymphocytic Leukemia
Experts Discuss Treatment Advances for Chronic Lymphocytic Leukemia
This article was originally published by Pharmacy Times
In the Pharmacy Times ® Directions in Oncology™ Insights series on chronic lymphocytic leukemia (CLL), experts Alison Duffy, PharmD, BCOP, and Cody Steeves, PharmD, BCOP, discussed current treatment recommendations and what is next for the disease state.
CLL is a rare cancer of the blood and bone marrow, and although it is difficult to treat many advances have been made in the past 6 years, said Duffy, an associate professor, clinical pharmacy specialty in oncology at the University of Maryland School of Pharmacy.
Earlier recommendations included single-agent chemotherapy or single-agent monoclonal antibodies, but Duffy explained that patients are increasingly receiving small molecule inhibitors, including Bruton tyrosine kinase (BTK) inhibitors.
Without the use of single-agent chemotherapies or single-agent monoclonal antibodies, Duffy said pharmacists can see patients with CLL in many settings.
“Using those as single agents, or more commonly in combination, that’s where the pipeline and future directions are really moving towards, with combination therapy as well as more potent, more selective, targeted therapies,” she said.
According to recommendations from the National Comprehensive Cancer Center (NCCN), Duffy said some current frontline treatment agents include ibrutinib, venetoclax plus obinutuzumab, acalabrutinib with or without obinutuzumab, and chemo-immunotherapy, when warranted.
Frontline therapies present various challenges, although Duffy said the treatment criteria has become less rigid.
“Some of the things that I would think about would be age, fitness, comorbidities such as atrial fibrillation, and renal function if I was going to give something like fludarabine within the FCR [fludarabine, cyclophosphamide, and rituximab] regimen,” Duffy said.
She added that considering patient preferences and clinical experiences is important. Some patients may not be great candidates for oral therapy due to a lack of access, finance, comfort level, or adherence challenges. Similarly, transportation might be an issue for patients receiving intravenous chemotherapy and should be considered.
“Moving forward, it’s positive to see that the outcomes, when they’re stratified by those patients with the deletions, still tend to trend in the positive direction for those patients with these newer oral therapies we’ve had over the past 5 or 6 years,” Steeves said.
The experts also turned their attention to minimum residual disease (MRD) testing and how it affects the use of limited duration therapy. MRD testing is particularly helpful for diseases that require stronger treatments, Steeves said. He explained that some data has found that obtaining a low or negative MRD corresponds with significantly increased progression-free survival compared with medium or high levels of MRD. However, patients receiving oral agents, especially single-agent BTK inhibition alone or with a CD20 inhibitor, are not expected to achieve MRD. Despite the lack of MRD, Steeves said these agents can be valuable.
“Even though we’re not seeing those deep remissions with MRD negativity, undetectable MRD, we certainly are still seeing a large benefit of using these agents without that,” Steeves said.
Steeves, clinical oncology pharmacist, Biologics by McKesson, also emphasized the importance of a patient-specific treatment plan. Some patients may want to take the drug for as short a period as possible, while others find that it does not disrupt their daily lives to a large extent because they are already receiving multiple medications.
Finally, Duffy and Steeves turned their attention to BTK inhibitor monotherapy for patients with newly diagnosed CLL. Ibrutinib, a new BTK inhibitor, was investigated in the RESONATE trial (NCT01578707), which found long-term benefit of the drug upon 6-year follow-up. The trial also established ibrutinib as the first-line choice for older patients and those without a 17P deletion, thereby demonstrating significant progression-free survival benefit among those high-risk subgroups. However, Duffy noted that ibrutinib is not for everybody.
“If you have a patient with uncontrolled atrial fibrillation, who has a high risk of bleeding that can’t be mitigated, or uncontrolled hypertension despite optimizing therapy management, ibrutinib wouldn’t be my first choice,” Duffy said.
Although the various treatments all need to be evaluated based on unique patient needs, the recent developments for the treatment of CLL are very promising and exciting, Duffy concluded.
“We’re getting to have a better understanding of CLL biology and some of the prognostic indicators,” Duffy said. “These new therapies allow for treatment without some of the traditional chemotherapy agents.”
THE PHARMACY TIMES® DIRECTIONS IN ONCOLOGY™ INSIGHTS SERIES ON CLL CAN BE VIEWED AT WWW.PHARMACYTIMES.COM/INSIGHTS.
CLL Advocates NZ Newsletter Issue 2
CLL Advocates NZ Newsletter Issue 2
A number of you will be familiar with and regularly reading HealthUnlocked and Patient Power, two patient support and networking services (based in the UK and US respectively) that cover CLL in detail.
For those not yet in the habit, I can recommend both websites to CLL patients, and their families and supporters. You can access both through our website on our useful links page here, or go directly to Patient Power here and HealthUnlocked here. Access is free.
HealthUnlocked is published daily, with ten articles in each edition, that are mainly personal stories and discussion among people with CLL, and also occasional reviews of CLL-related clinical studies.
One such study, in the 20 July edition was on CLL and Covid 19. It provided an analysis of the assessment of 190 patients with CLL who had proven Covid 19 infection. Most presenting for analysis (79%) were in the “severe” category (requiring ICU admission and/or oxygen). This is likely to be related to their having had contact with a hospital. One third of these patients died of Covid 19. The severe group were older than the less severe group, so increasing age is a risk. There was a reduced rate of severe disease in those patients who had had treatment recently as opposed to those who had treatment remotely, or never.
Patient Power (PP) sends email updates to subscribers, generally weekly. Their CLL articles tend to have more of a scientific and medical focus. They also regularly post videos of interviews conducted by the PP CEO, Andrew Schorr, who is a long-term CLL survivor. He interviews well known clinicians on aspects of CLL, including the latest research and developments in the understanding and treatment of CLL. His wife, Esther, also writes regularly for PP.
An interesting recent PP article discussed CAR T-cell treatment, which is being trialled for CLL in research centres globally, including the Malaghan Institute in Wellington (Dr Rob Weinkove).
As an aside on CAR T-cell therapy, I recently enjoyed a book by NZ comedian David Downs on his experience with cancer (in his case, lymphoma). The book is entitled “A Mild Touch of the Cancer”. It is humorous and insightful on living with a serious health issue, and I commend it to you.
Finally, if you haven’t already seen it, check out our message on Facebook and on our website about our first CLL education event, to be held in Auckland, on Wednesday 14 October 2020. The event will be jointly hosted with Leukaemia & Blood Cancer. For those unable to be there in person, you’ll be able to join us via Zoom, to hear talks by and discussion with three of our country’s foremost CLL clinicians. As well as providing the latest information on CLL we hope to extend our reach and ability to support people living with CLL, and I warmly encourage you to help spread the word and attend the event with your family and supporters. More detail on the event including how to register will be circulated soon.
With best wishes
Neil Graham FRACP, FRCP
Executive Director
CLL Advocates NZ
CLL Experts Favor Social Distancing, but Vary on Treatment Continuation Amid Pandemic
CLL Experts Favor Social Distancing, but Vary on Treatment Continuation Amid Pandemic
This article was originally published by AJMC
The survey is the latest attempt to figure out how best to manage patients with CLL amid the pandemic, given that patients with the cancer tend to be older in age, have comorbidities, and be immunosuppressed.
In a letter to the editor of the American Journal of Hematology, corresponding author Mazyar Shadman, MD, MPH, of the Fred Hutchinson Cancer Research Center, in Seattle, and colleagues reported on a survey sent to 62 CLL specialists in the United States, Canada, Europe, and Australia. Of those, 59 responded to at least 1 question, and 44 completed the entire survey.
When asked about social distancing recommendations for patients with CLL, 32% said they would advise patients to follow the same guidelines as the WHO and Centers for Disease Control and Prevention (CDC) recommend for the general public. Twenty-one percent said they would advise patients to follow those guidelines but also limit regular outings by asking friends to pick up groceries or medications for them. Another 35% went even further, saying patients with CLL should avoid work, even if they are essential workers. The remaining 12% said they would recommend all of the above, plus wearing N95 masks and gloves outside of the house.
In terms of testing, most experts said it was not necessary to test all patients with CLL for COVID-19. Specifically, 62% of experts said they would limit testing to patients who call to and report symptoms, and another 9.5% said tests should be limited to patients who come in for an office visit and report symptoms.
Still, while clinicians generally had a low bar for what types of symptoms warranted testing. “Most favored testing patients with any levels of reported symptoms, even with limited testing availability,” Shadman and colleagues wrote. “With unlimited access, 23% recommended universal testing.”
Though their approaches to social distancing and testing were in line with recommendations for the general public, the experts expressed caution when it came to continuation of outpatient therapy. Only 14% said CLL therapy should be continued unconditionally. Most (60.5%) favored treatment discontinuation, and 25.5% said they favored continuation only based on the specific clinical situation.
However, when it came to bruton tyrosine kinase inhibitors (BTKis), such as ibrutinib (Imbruvica) and acalabrutinib (Calquence), the proportion of experts favoring unconditional treatment continuation was much higher, at 44%.
Shadman and colleagues said the more favorable responses concerning BTKi continuation may be due to concern about disease flares if treatment were stopped.
“Also, there is a theoretical benefit of BTKi’s in blunting the hyperinflammatory stage of COVID-19 disease by targeting macrophages and/or inhibiting pro-inflammatory cytokines,” they said.
Most experts (72%) recommended against the use of intravenous immune globulin (IVIG), though the authors noted that the survey was conducted in late March and early April, “before passive antibodies in the gammaglobulin pool would be expected.”
Shadman and colleagues said additional study is warranted to better understand the optimal approach to management of patients with CLL during the pandemic.
A 79-Year-Old Man With Relapsed Chronic Lymphocytic Leukemia
A 79-Year-Old Man With Relapsed Chronic Lymphocytic Leukemia
This article was originally published by Targeted Oncology
High-Risk Chronic Lymphocytic Leukemia
Jeff Sharman, MD: Hello, my name is Jeff Sharman. I’m the Medical Director of Hematology Research for US Oncology, and I am a practicing oncologist at the Willamette Valley Cancer in Eugene, Oregon.
Today I’ve been asked to present a case of a 79-year-old gentleman with relapsed chronic lymphocytic leukemia to address some of the treatment considerations we have in this patient population.
This particular patient is a hypothetical patient but referred to me. We’ll say that he was a 79-year-old gentleman who initially presented to his outside medical oncologist for the first time complaining of some vague intermittent abdominal pain and progressive fatigue. His past medical history is notable primarily for medically-controlled hypertension. He had a myocardial infarction 8 years ago and is on low-dose aspirin. His original CLL diagnosis was about 7 years ago, and after a period of watchful waiting, he had progressive lymphocytosis and adenopathy. He was treated with ibrutinib 420 mg daily, his symptoms improved, and he achieved a stable disease with resolution of lymphadenopathy.
Unfortunately, after 5 years of disease control on ibrutinib, he complained of increasing fatigue and decreasing appetite. Upon physical exam, he had a return of palpable lymphadenopathy, and his spleen was palpable, 4 centimeters below the costal margin. At that time, seen by an outside medical oncologist, he was started on rituximab monotherapy due to his medical comorbidities, but after 6 months on this regimen, he presents to my clinic after moving to be closer to family.
His physical exam was notable this time for palpable bilateral cervical adenopathy, right-sided inguinal adenopathy. Labs showed a white blood cell count of 55,000, predominately lymphocytes, and neutrophil count of 3100. He was anemic and thrombocytopenic, with a hemoglobin of 9.4 and platelets of 90,000, respectively. His beta-2 microglobulin was elevated, and, notably, he had a creatine clearance of just 31 mL per min.
Flow cytometry confirmed the typical immunophenotype for CLL, and at this time, FISH testing was performed and, importantly, returned a deletion of 17p in a high fraction of the cells. He was Rai stage 4 with an ECOG performance status of 1. At this time, treatment was initiated with idelalisib in combination with rituximab, or I should say idelalisib was added to rituximab at this time, 150 mg PO BID.
Now this is an interesting case, and it presents a number of features that are challenging in terms of how to pick therapy in this population with significant comorbidities. I’ve been asked to address questions pertaining to both his prior management, his current situation, and so forth.
The first question I’ve been asked is to describe my initial impression of the case and what the prognosis was for this patient. You know this is a patient who has high-risk CLL. He has relapsed after ibrutinib, and he has a deletion of 17p. What that means is that chemoimmunotherapy is not going to work for this individual, so you really don’t have that much in the way of options. Then you’ve exhausted BTK inhibitors, and there’s a question of what you have left.
In this particular case, the outside provider used rituximab monotherapy probably for lack of clarity in what options might have been available; this is a patient that because of his age and comorbidities, it’s very possible this patient may ultimately pass away of their CLL, which, in contemporary CLL management, seems like a relatively rare occurrence.
When we discuss risk stratification for patients with chronic lymphocytic leukemia, there’s a couple of things that are really important. We think about their IgHV status, which is really a measurement of how quickly the CLL is growing. What are the kinetics of growth? Then we think about the FISH status, which is how resistant it is to therapy. Deletion of 17p is a particularly noteworthy abnormality because patients with 17p have very brief responses to chemoimmunotherapy-based approaches.
Similarly, we’re seeing updates with targeted therapy, such as venetoclax, that 17p can retain adverse prognostic significance in this population. In this particular patient’s case, idelalisib had been added to the regimen. It’s noteworthy that idelalisib outcomes appear to be independent of 17p, so whether 17p is present or not, the outcomes relative to 17p don’t matter quite as much.
Transcript edited for clarity.
Case: A 79-Year-Old Man With Relapsed Chronic Lymphocytic Leukemia
Initial presentation
- A 79-year-old man presented to a new medical oncologist for the first time complaining of vague intermitted abdominal pain, and progressive fatigue
- PMH:
- Hypertension, medically controlled
- MI, 8 years ago, on 81 mg aspirin
- CLL, diagnosed 7 years ago
- After a period of watchful waiting he began treatment with ibrutinib 420 mg PO qDay; symptoms improved and achieved stable disease, resolution of lymphadenopathy
- After 5 years of disease control on ibrutinib he complained of increasing fatigue and decreased appetite, on physical exam there was return of palpable lymphadenopathy; spleen was palpable ~4 cm below costal margin
- He was started on rituximab
- Currently after 6 months on rituximab monotherapy he presents to the clinic
- PE: palpable bilateral cervical and right-sided inguinal lymphadenopathy
Clinical workup
- Labs: WBC 55,000, lymphocyte 82%, ANC 3100/mm3, Hb 9.4 g/dL, plt 90 x 109/L, LDH 220 U/L, Beta-2-microglobulin 3.9 mg/L; creatinine clearance 31 mL/min
- FC CD 5+, CD19+, CD20+ monoclonal B-cell population
- FISH: CLL probe set tested, deletion 17p
- IgHV mutational status: unmutated
- Rai stage IV; ECOG PS 1
- Treatment of idelalisib 150 mg PO BID was added to rituximab
Age, Recent Treatment, Appear to Influence Severity of COVID-19 in Patients With CLL
Age, Recent Treatment Appear to Influence Severity of COVID-19 in Patients With CLL
This article was originally published by AJMC
Patients with chronic lymphocytic leukemia (CLL) who contract coronavirus disease 2019 (COVID-19) face more severe symptoms if they are older, though recent treatment with antileukemic agents appears to have a beneficial, rather than detrimental, effect on outcomes, a new study found. The study also suggests that the presence of comorbidities does not lead to higher mortality rates.
The retrospective analysis is based on 190 patients with CLL who had confirmed COVID-19 cases between late March and late May. The results were published in the journal Leukemia.
Corresponding author Kostas Stamatopoulos, MD, PhD, of the Center for Research and Technology Hellas, in Greece, wrote along with colleagues that CLL is a “paradigmatic example” of a malignancy that has been associated with impaired immune responses to pathogens, which they said could have negative impacts on outcomes when patients with CLL contract COVID-19. The investigators added that antileukemic treatments could further hamper the immune system’s ability to fight off a virus like SARS-CoV-2, though they said it’s not a straightforward proposition.
“On the other hand, the severity of COVID-19 and [multiorgan failure] occurrence seem to be related to clinical and laboratory parameters of inflammatory response (lymphopenia, hypoalbuminemia, higher levels of alanine aminotransferase, lactate dehydrogenase, C-reactive protein, ferritin, and D-dimer) and markedly higher levels of proinflammatory cytokines (interleukin-2 receptor, IL6, IL-10, and tumor necrosis factor-α),” they said. “On these grounds, therapies targeting inflammation (eg, IL6/IL6R antibodies or steroids) have been used and shown potential benefit in full-blown COVID-19 patients.”
In an effort to ascertain a real-world understanding of what patients with CLL who contract the virus should expect, Stamatopoulos and colleagues analyzed the 190 colleagues based on age, gender, and comorbidities; severity of COVID-19; and whether and how long ago they had been treated with antileukemic therapies.
The investigators found a strong majority (151, or 79%) of patients presented with severe symptoms, such as requiring oxygen or admission to an intensive care unit. Patients were more likely to have severe symptoms if they were aged 65 or older.
Recent treatment appeared to make a significant difference. Only 4 in 10 patients with severe symptoms had received antileukemic treatment within the past 12 months. However, among those with mild symptoms, 76.9% had undergone recent treatment. Among those with severe symptoms, the likelihood of hospitalization was lower if they had received therapy with ibrutinib (Imbruvica).
More than one-third (36.4%) of patients with severe symptoms died from COVID-19; versus just 1 of the 38 patients with mild symptoms succumbed.
Stamatopoulos and colleagues noted that the apparent link between age and mortality among patients with CLL tracks with known data from the general population. However, they said comorbidities did not appear to have a significant impact on whether a patient had mild or severe symptoms.
As for the impact of antileukemic therapies, the authors said a disproportionate percentage of their study population had been prescribed bruton kinase inhibitors. Thus, they did not have sufficient data to compare the impact of BTK inhibitors to other types of therapy.
Still, they said their data seems to support the idea that recent antileukemic therapy is beneficial against COVD-19.
“Altogether, these data seem to further underscore the possible protective role of specific targeted therapies against a dismal evolution of the SARS-CoV-2 infection,” they said.
Tool appears to predict need for treatment in asymptomatic, early-stage CLL
Tool appears to predict need for treatment in asymptomatic, early-stage CLL
This article was originally published by Healio
A novel prognostic tool appeared to predict the need for treatment among patients with asymptomatic, early-stage, chronic lymphocytic leukemia, according to research published in Blood.
“CLL is an indolent disease that is treated only if symptomatic. Currently, between 70% and 80% of newly diagnosed [patients with CLL] are asymptomatic and therefore are offered a wait-and-see approach to management consisting of regular visits every 3 to 12 months. However, this approach is not easily accepted by patients, who often ask whether, when and how they will be treated,” Davide Rossi, MD, researcher at Oncology Institute of Southern Switzerland, told Healio. “So far, the eventual disease course cannot be predicted for patients after they have been offered wait and see, which in turn causes anxiety and uncertainty. Having a tool that accurately forecasts leukemia course will help patients in planning their life with the disease.”
Rossi and colleagues developed and tested the international prognostic score, IPS-E, to predict time to first treatment among 4,933 patients with early-stage, asymptomatic CLL included in 11 global cohort studies.
Among a training cohort of 333 patients, investigators observed three consistent and independent covariates that appeared associated with time to first treatment: unmutated IGHV genes, absolute lymphocyte count greater than 15 x 109/l and the presence of palpable lymph nodes. They used data from this cohort to develop a prognostic score with each factor counting as one point. Patients with zero factors were considered at low risk for requiring treatment within the first 5 years of diagnosis, those with one factor were considered at intermediate risk, and those with two or three factors were considered at high risk.
Investigators validated the score in nine cohorts staged by the Binet system and in one study staged by the Rai system. They observed C-index scores of 0.74 in the training series and 0.7 in the aggregate of validation series.
Overall, approximately 30% of patients were categorized as low risk, 35% as intermediate risk and 35% at high risk.
Moreover, meta-analysis of the cohorts showed 5-year cumulative risk for treatment initiation of 8.4% among patients considered low risk, 28.4% for those in the intermediate-risk group and 61.2% for those at high risk.

“In a time where the treatment paradigm of asymptomatic CLL may change if a survival benefit is proven by early intervention with novel agents, our international prognostic score could help in defining the early-stage population where treatment can be appropriate,” Rossi said. “Moreover, it could be helpful for the treating physician to better allocate medical resources, such as deciding on the interval between clinical assessments according to risk group. Health care professionals will be supported in the discussion while explaining CLL to patients — many of whom have never heard about the rare tumor. Physicians can also safely plan and advise in advance the proper timing of surveillance visits according to the predicted risk of leukemia progression.”
The international prognostic score warrants prospective evaluation, according to Rossi, and can be regarded as a building block on which newly discovered independent outcome predictors for patients with early-stage CLL could be added.
“In this sense, a prospective study could be designed to further assess and eventually strengthen this prognostic tool,” Rossi said.
For more information:
Davide Rossi, MD, can be reached at Oncology Institute of Southern Switzerland, Via Ospedale, 6500 Bellinzona, Switzerland; email: davide.rossi@eoc.ch.
Changes in Management of CLL Due to COVID-19 Noted in Italy
Changes in Management of CLL Due to COVID-19 Noted in Italy
This article was originally published by Cancer Therapy Advisor.
The clinical management of patients with chronic lymphocytic leukemia (CLL) was altered across Italy in response to the COVID-19 pandemic, according to a survey study published in Blood.
“What is starting to emerge is an impact on the routine work-up of patients, on treatment choices, and the enrollment and adherence to clinical trials,” the authors wrote.
The authors sent a survey to 33 hematology centers across Italy in early April that included questions about testing strategies for COVID-19; the effect of the pandemic on diagnosis, management, and the outcomes of patients with CLL; and the adherence to clinical protocols. The survey data was based on 9930 patients with CLL, which represents approximately one-third of all patients with CLL in Italy.
Although the minimum testing requirements mandated by law were followed by all centers, only 30% of centers tested asymptomatic patients without any known contact with a COVID-19 case prior to initiating CLL treatment. The authors said that this “reflects the higher capacity of some regional health systems to performed analyze nasopharyngeal swabs.”
CONTINUE READING
Of the 9330 patients with CLL, 47 (0.5%) patients were symptomatic and tested positive for COVID-19.
Most centers reported a decrease in the number of newly diagnosed CLL cases, likely due to a decrease in the use of peripheral laboratories for diagnostic work-up, the authors said. In addition, 15.2% of centers reported that delays and difficulties in an accurate diagnostic work-up has occurred due to a reduction in personnel.
New treatment initiation was delayed in 79% of centers, and 24% of centers reported a delay in ongoing therapy. Delayed post-treatment restaging also occurred in 30.3% of centers.
The sample size was not large enough to characterize patient outcomes due to COVID-19 or the effect of anti-CLL treatments. However, there was a mix of patients who were receiving active first-line or salvage treatment vs no active treatment.
The mortality rate in this cohort was 30.4%. “The mortality rate for symptomatic COVID-19 patients amongst the general population was 13.4% and 25.5% in the 70- to 79-year-old population,” the authors noted.
Clinical trial enrollment and follow-up of patients on a clinical trial protocol was reduced in two-thirds of the centers.
The authors concluded that this survey has revealed that COVID-19 “has started to impact on the number of new cases, on the adequate follow-up of treated patients, on the number of patients enrolled in clinical trials, and on the monitoring of such patients.”
Specialty Pharmacists Have Broad Responsibilities in Chronic Lymphocytic Leukemia
Specialty Pharmacists Have Broad Responsibilities in Chronic Lymphocytic Leukemia
This article was originally published by Pharmacy Times.
AT JUST 1.2%, chronic lymphocytic leukemia (CLL) represents a small percentage of all new cancer cases but is the most common leukemia in Western countries. In 2019, oncologists diagnosed an estimated 20,720 new cases and approximately 3930 people died. One virtual symposium held in conjunction with the Asembia Specialty Pharmacy Summit explored this cancer, which most often occurs in older adults.
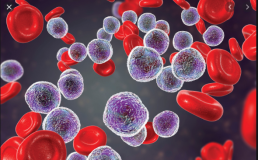
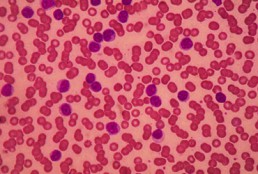
Alison Duffy, PharmD, BCOP, presented a comprehensive overview. Patients with CLL experience a gradual, malignant accumulation of lymphocytic blood cells that begins in the bone marrow and eventually extends to the blood. Genomic alterations cause leukemic transformation that inhibits apoptosis of clonal B cells. Del(17p) is the most important prognostic factor, reflecting the loss of a key tumor suppressor gene.
Oncologists generally begin treatment when patients’ end organ function is threatened, or they have progressive bulky disease, extensive adenopathy, or splenomegaly. Other factors that may signal a need for treatment are progressive bone marrow failure, constitutional symptoms, autoimmune anemia, leukostasis, or increasing absolute lymphocyte count. Those who are at least 65 years of age or who are younger and frail are treated in a “go slow” manner, whereas patients who are younger than 65 years with no significant comorbidities can be treated more aggressively.
Duffy discussed the evolving treatment paradigm of CLL, underscoring that therapy selection and patient management are complex. She focused on the small-molecule oral agents, including acalabrutinib, duvelisib, ibrutinib, idelalisib, and venetoclax, as well as evidence for their use in combination strategies. She demonstrated how each affects pathogenic pathways in CLL and also differentiated between treatment algorithms for naïve CLL and relapsed/refractory CLL. Ibrutinib and venetoclax are both approved as single agents in the first line, but other first-line therapies are combinations of acalabrutinib with obinutuzumab and venetoclax with obinutuzumab.
Duffy finished her presentation by discussing novel therapies currently in clinical trials and future implications. A number of other agents, both smallmolecules and monoclonal antibodies, are currently in clinical trials either alone or in combination with existing drugs.
Kirollos S. Hanna, PharmD, BCPS, BCOP, emphasized multidisciplinary collaboration with the fact that pharmacy-led chemotherapy management programs can improve 5 aspects of care:
- Patient knowledge
- Patient adherence to therapy and clinician adherence to prescribing standards
- Time to medication access
- Identification of clinically significant issues
- Provider and patient satisfaction
Hanna indicated that common standards of care exist for infection prophylaxis. He shared prophylactic recommendations for Pneumocystis jirovecii pneumonia, herpes simplex virus, cytomegalovirus, and hepatitis B related to use of specific agents.
Specialty pharmacists need to be closely involved with management of adverse effects (AEs). Hanna noted that AEs are the most common reason for kinase inhibitor discontinuation. He reviewed each agent’s most common AEs and suggested clinical interventions.
Hanna emphasized the importance of a medically integrated model. He discussed the 3 stages of treatment: (1) initiation, (2) coordination, and (3) maintenance, indicating that certain actions are “operational best practices.” A patient education checklist that he presented emphasized all of these points.
Finally, he highlighted the consequences of failure to access these costly agents. Prescription abandonment, poor adherence, treatment delay, decreased quality of life, and suboptimal disease outcomes are problematic for patients. He urged pharmacists to investigate benefits early in the process, have patients engage with assistance teams and counselors, look at every available co-pay assistance program, explore free drug programs, and integrate the financial team into the multidisciplinary process.
Discontinuation of Venetoclax Impacts Outcomes of Rituximab Combination in CLL
Discontinuation of Venetoclax Impacts Outcomes of Rituximab Combination in CLL
This story was originally published on Targeted Oncology
In an interview with Targeted Oncology, Anthony Mato, MD, discussed the findings of venetoclax interruptions or discontinuations observed in patients with relapsed/refractory chronic lymphocytic leukemia who received the combination of venetoclax plus rituximab in the phase 3 MURANO study.
Early discontinuation of venetoclax (Venclexta) was associated with suboptimal outcomes in an analysis of patients with relapsed/refractory chronic lymphocytic leukemia (CLL) in the phase 3 MURANO clinical trial, which was presented during the 2020 American Society of Clinical Oncology (ASCO) Virtual Scientific Program. These findings demonstrate the importance of effective management of adverse events (AEs) for patient to experience the full benefit of the combination venetoclax plus rituximab (Rituxan).
Discontinuation or dose interruptions of venetoclax appear to occur frequently in this patient population. This analysis aimed to evaluate how discontinuation or dose interruptions impact outcomes in this patient population.
Out of 194 patients, 140 completed 2 years of the combination regimen; 54 patients discontinued treatment early due to AEs in 29, disease progression in 12, withdrawal in 5, physician’s decision in 3, death in 2, noncompliance in 1, and for other reasons in 2. The median duration of venetoclax in patients who discontinued due to AEs was 11.3 months (range, 0.5-24.6) and 17.1 months (range, 4.6-25.1) for those who discontinued due to progressive disease (P =.08).
Inferior progression-free survival (PFS) was noted in patients who discontinued venetoclax early for any reason except for progressive disease or AEs compared with those who were able to complete treatment. Greater exposure to venetoclax cumulatively reduced the risk significantly of a PFS (HR, 0.93; 95% CI, 0.88-0.99; P =.0168) or overall survival (OS) event (HR, 0.85; 95% CI, 0.79-0.92; P =.0001).
Interruptions due to AEs occurred in 134 patients, which were mostly due to neutropenia (43%). The median duration of venetoclax interruptions was 9 days (range, 1-93). Interruptions did not have an impact on PFS or OS
In an interview with Targeted Oncology, Anthony Mato, MD, director of the Chronic Lymphocytic Leukemia Program, Memorial Sloan Kettering Cancer Center, discussed the findings of venetoclax interruptions or discontinuations observed in patients with relapsed/refractory CLL who received the combination of venetoclax plus rituximab in the phase 3 MURANO study.
TARGETED ONCOLOGY: Could you begin by providing some background on this study?
Mato: The MURANO trial is a trial comparing the combination of venetoclax and rituximab given for a total of 24 months, where the rituximab is given for 6 months and the venetoclax is given for a total of 2 years as compared to bendamustine/rituximab, which is a commonly used chemoimmunotherapy combination in the frontline and relapsed/refractory settings. The trial was conducted several years ago. Now we have 4 years follow up and initially and has subsequently demonstrated success in terms of the primary endpoint, in terms of PFS, as well as an OS advantage, favoring the venetoclax-based therapy, representing a paradigm shift in the management of patients with relapsed/refractory disease, in that we have a new molecule which rivals over a known standard of care, as well as a time-limited therapy approved in the relapsed/refractory setting.
TARGETED ONCOLOGY: Could you shed light on the methods that were used to conduct this particular analysis?
Mato: The analysis that was presented at the ASCO meeting is trying to address the question about whether or not outcomes are impacted for patients who have to undergo dose reductions, dose interruptions, and also for the small subset of patients who discontinue the time-limited therapy prior to the 24 months planned end point for continued therapy. Here we were looking at outcomes, particularly PFS, and how those particular factors might impact the primary end point of the MURANO trial for again, the small subset of patients who did require interruptions, reductions, and early or premature discontinuation.
TARGETED ONCOLOGY: What were some of the main reasons for discontinuing or interrupting treatment with venetoclax?
Mato: In most of the novel agents that have been approved for CLL, there’s always 2 competing factors that seem to lead to most of the dose reductions or interruptions and/or discontinuation, and those always seem to include AEs or progression of disease.
TARGETED ONCOLOGY: What do the results show in terms of the impact on outcomes?
Mato: The take home message from this trial is that it’s really best to try to understand how to use the label of venetoclax effectively to maintain continuous dosing for the 24 months. If patients required brief interruptions or dose reductions to try to find that right balance between AEs and continued exposure to this active agent, they were able to do just fine, and there was no significant impact on the outcomes. For patients who had to discontinue early, , those patients did have an impact on their outcomes. The lesson learned here is that if a patient requires a dose reduction due to neutropenia or diarrhea for example, it’s better to understand the label and appropriately apply supportive care and to dose reduce, rather than to just give up on using the combination all together.
TARGETED ONCOLOGY: Could you elaborate on what those supportive care measures would entail?
Mato: It depends on the AE. Frequently, in clinical practice, if a patient experiences neutropenia, for example, which is probably the most common AE, one can use growth factors like filgrastim (Neupogen) or pegfilgrastim (Neulasta) to support the white blood cell count. Fortunately, with venetoclax, you don’t need a lot of growth factor in order to maintain an absolute neutrophil count of about 1000, so sparing use once or twice a week might do it to maintain a dose of 400 mg. If the patient continues to experience neutropenia, then one might consider also reducing the dose from 400 mg, for example, to 300 mg or 200 mg. That might be 1 strategy.
Another supportive care measure is working with a clinical pharmacist to verify that there aren’t particular medication interactions that might increase the venetoclax dose or level such that you may experience AEs. Patients who have diarrhea, for example, might benefit from a brief hold, a dose reduction, a brief interruption, or use of supportive care. Like with any novel agent, there’s a learning curve associated with use of venetoclax, but once you’re able to understand the AEs, which are fairly predictable and it’s not like there’s hundreds of AEs associated with this drug, you can come up with measures related to dose reductions, interruptions, or adding in medications or supportive measures that allow patients to stay on drug.
TARGETED ONCOLOGY: Is there anything else you wanted to emphasize?
Mato: It’s important that these types of analyses are conducted when exploring the use of novel agents after the initial results of key trials are reported, particularly with the BTK inhibitors. We’ve seen similar types of analyses conducted, as well as less so with the Pi3K inhibitors, but I think it does provide an important framework for those practicing and taking care of patients who may require these types of measures in order to stay on drug to really help provide reassurance that outcomes are not compromised if you’re following the label and are able to stay on drug at a dose that’s right for a particular patient.
CLL Advocates NZ Newsletter Issue 1
CLL Advocates NZ Newsletter Issue 1
Welcome to our first CLL Advocates newsletter. Like many organisations, we weren’t able to accomplish very much over the lockdown period. We did, however, manage a Trustees’ teleconference to shape up our strategy for the next 12 months. One of the proposals made at that meeting was a monthly newsletter, so here is the first edition.
A huge number of lay and medical articles have been written about the COVID pandemic, and, as you may have seen on our website, we’ve published a number relevant to people living with CLL. See them here. One of particular interest was a consensus statement by Australasian haematologists on management of blood cancers in the COVID pandemic (published in May’s Internal Medicine Journal). It noted that, with a mean age of diagnosis of about 70 years, CLL patients are already likely to be in a high-risk group simply because of age. Advice specifically directed to CLL patients was:
- to delay planned therapy where possible
- to consider using oral agents over IV medications so as to avoid exposure to higher risk environments such as hospital chemotherapy units, for treatment of both initial therapy, and for relapsed/refractory disease (see our recent letter to Pharmac on this matter).
New Zealand has done extraordinarily well at this stage to contain the virus, though it should be noted that vaccination, if successfully developed, may present further challenges for CLL patients.
The CLLANZ Trustees’ meeting agreed that information/education initiatives on CLL should be high on our priority list. In this regard, a review of the current management of CLL by Dr Gillian Corbett, haematologist and trustee, has been published on our website. A detailed CLL patient information booklet is also now close to sign-off and will be published shortly.
In October this year we will be staging a half day or evening combined meeting/seminar on CLL in NZ with the Leukaemia & Blood Cancer (LBC) group, with leading NZ CLL specialists. This will be ‘in person’ in Auckland and also online on Zoom so that people from around the country can join in the discussion and if desired put questions to the speakers. Details will follow soon.
To ensure we reach as many people as possible who have an interest in CLL, we encourage you to become a ‘friend’ of CLL Advocates NZ – by signing up to our newsletter here and/or joining our private Facebook group. You can apply to join the group here.
More details of anticipated activities will follow in subsequent newsletters.
Meanwhile, now that we have passed the winter solstice, and are becoming adjusted to the new ‘normal’, stay well, physically, mentally and spiritually. And please remember that as well as our advocacy role, we want to be a source of knowledge and support for New Zealanders living with CLL, and their families and supporters. To help us achieve this we would welcome and appreciate your feedback, and your thoughts on how we can best achieve our mission.
With best wishes
Neil Graham FRACP, FRCP
Executive Director
CLL Advocates NZ