Clinical Trials for Chronic Lymphocytic Leukaemia
Clinical Trials.
In New Zealand, individuals diagnosed with Chronic Lymphocytic Leukaemia (CLL) have some options when considering clinical trials.
Patients can explore trials aiming to improve outcomes and quality of life for those with CLL. Additionally, New Zealand's participation in international collaborations provides access to a diverse range of clinical trials, offering patients the opportunity to contribute to cutting-edge research while potentially accessing innovative treatments.
Note:
If a study is not open in your area, discuss with your Haematologist if you can be referred to a centre where it is open.
Centres will usually consider cross referrals, although it will mean some travel.
Sometimes for commercial studies the cost of travel and accommodation may be paid.
Please click on this link, Clinical_ Trials for information on available trials
Added support for use of Brukinsa in relapsed or refractory CLL/SLL
An interesting study on a drug, Brukinsa that is not yet in New Zealand, although we and Australia had 9% of patients enrolled in the trial. Hopefully the drug will make it to New Zealand at some stage in the future.
"China-based biotech BeiGene (HKEX: 06160) has announced results from the Phase III ALPINE trial showing BTK inhibitor Brukinsa (zanubrutinib) demonstrated superiority versus ibrutinib in overall response rate (ORR) as assessed by an Independent Review Committee (IRC) in adult patients with relapsed or refractory (R/R) chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
A total of 652 patients were enrolled in the ALPINE trial across:
Europe (60%) ; USA (17%) ; China (14%) ; New Zealand and Australia (9%) and were followed for a median of 24.2 months. The next planned analysis of ALPINE data will be the PFS final analysis.
Brukinsa, which is cleared in markets such as the European Union, USA, China, Brazil and Canada for the treatment of marginal zone lymphoma (MZL) and mantle cell lymphoma (MCL) in some markets.
BeiGene has submitted results from the ALPINE trial in support of marketing authorization applications for Brukinsa in CLL in the USA, EU and other markets around the world. In February 2022, BeiGene announced that the US Food and Drug Administration and European Medicines Agency have accepted supplemental new drug applications for Brukinsa in CLL".
For more information on the trial, please click on this link: Added support for use of Brukinsa in relapsed or refractory CLL/SLL (thepharmaletter.com)
Blood type may predict which cancer patients are prone to clots
Cancer and its treatments increase the risk for venous thromboembolism (VTE). That includes deep-vein thrombosis (DVT, a blood clot that typically forms in the deep veins of the leg) and pulmonary embolism (PE, a life-threatening condition that occurs when a blood clot breaks free and travels to the lungs' arteries).
Factors such as tumours or cancer types are now used to identify cancer patients at high risk of VTE, but many go unidentified. This study concluded that cancer patients with non-O blood types, such as types A, B and AB, are at increased risk for VTE.
For more information please click on the link: Blood Type May Predict Which Cancer Patients Are Prone to Clots - Consumer Health News | HealthDay
CLL Horizons 2021 - 5-7 November 2021 - Register Now!
CLL Horizons 2021 - 5-7 November 2021 - Register Now!
The CLL Advocates Network (CLLAN) Steering Committee is pleased to announce the 4th international CLL Horizons Conference which will be held in a fully virtual format.
REGISTRATION IS NOW OPEN! Please REGISTER HERE to join us online at CLL Horizons 2021 (CLLHZ 2021) from 5-7 November!
The CLL Horizons Conference is a unique opportunity for patient advocates and patient organisation representatives supporting CLL patients to:
· Learn about the disease, treatments and latest research from leading doctors
· Hear from fellow advocates on key topics, including awareness, education and drug access
· Network virtually with others doing similar work, giving them the opportunity to discuss issues facing CLL patients.
You will gain important knowledge that will help you improve your support of CLL patients in your community.
The 3-day conference will be conducted in English, and some sessions will be duplicated to allow participation of attendees joining from the Southern Hemisphere.
The conference includes topics of importance to the CLL patient community and provides a unique opportunity for participants to share experiences and best practice. We have again been able to attract renowned experts and speakers from different parts of the world, such as Prof Florence Cymbalista from France, Prof Con Tam from Australia or Prof Anna Schuh and Dr. Talha Munir (both from UK). You will find interesting medical and advocacy sessions as well as plenty of interactive panel sessions.
The platform offers an exhibition space for groups to showcase their activities, materials and projects. You will also be given the opportunity to submit a poster on any general CLL advocacy support activity of your choice as well as to submit abstract on a best practice example around “The impact of the pandemic on Patient Organisations – best practice examples of transforming challenges into opportunities.” Three abstracts will be selected and winners will get the opportunity to present these in our “Hear from the regions” on Day 2. More details will be shared once you have registered.
You can access a top-line conference agenda HERE!
If you are curious to learn more about previous Horizons conferences, access the videos of sessions held in prior years and read the conference summary reports, please check out the “Go to previous CLL Horizons Conferences“ at the bottom of the CLLHZ section on our website.
And now REGISTER FOR CLL HORIZONS 2021 HERE!
Should you have questions, please do not hesitate to get in touch with our Event Manager, Natasha Sambhi at natasha@successful-events.co.uk. Natasha will be happy to help you with your questions.
We look forward to seeing you (virtually!) in November!
Living with CLL
Living with CLL
Please watch the video on
WHAT IS THE DIFFERENCE BETWEEN CLL AND SLL?
By Dr Rob Weinkove (Haematologist)
Pharmac commits to being more transparent
Priority lists for funding applications
On 28 July for the first time Pharmac released its ‘Options for investment list’. These are the priority medications Pharmac would like to fund if they had the budget to do so. They do not provide a ranking so we don’t know where each medication sits on the list. See the list here.
As a Cancer Patient, Will I Need an Extra Dose of a COVID-19 Vaccine?
As a Cancer Patient, Will I Need an Extra Dose of a COVID-19 Vaccine?
This article was originally posted on Patients Power
Individuals who are immunocompromised, including people with cancer, are wondering if they will need an additional dose of a COVID-19 vaccine to increase their level of protection against the coronavirus. The Advisory Committee on Immunization Practices (ACIP), which makes recommendations to the Centers for Disease Control and Prevention, met on July 22 to discuss this issue, among other topics. The meeting was a preliminary step in discussing the safety and effectiveness of additional vaccine doses before any new recommendations can be made.
When a person has cancer, there are two main reasons why they have an increased risk of infection: Either the disease itself or its treatment may cause suppression of the immune system. When this happens, a person may be considered immunocompromised. It is estimated that close to 3% of the U.S. population is immunocompromised, including those with solid tumors and blood cancers, people who have had organ or stem cell transplants, and those being treated with drugs that affect the immune system, including certain chemotherapy medications and corticosteroids.
While research indicates a very strong response to the COVID-19 vaccines in the general population, there is growing evidence that some people who are immunocompromised have a less robust immune response, even after they have been fully vaccinated.
Let’s review a bit. With rare exceptions, it is vital for everyone with cancer to get a COVID-19 vaccination as soon as they can, including those on most active treatments. Many experts at the ACIP meeting reemphasized the importance of vaccinations for people who are immunocompromised and further pointed out the key role of a “circle of protection” surrounding those who are immunocompromised consisting of other vaccinated individuals. It is important that all household members and others you are in close contact with are vaccinated.
Is there a link between CLL and stomach pain?
Is there a link between chronic lymphocytic leukemia and stomach pain?
This article was originally posted on Medical News Today
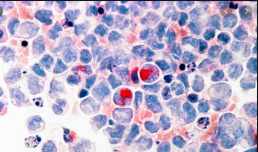
Chronic lymphocytic leukemia (CLL) is a type of blood cancer. It affects lymphocytes, a type of immature white blood cell that the body produces in the bone marrow.
People with CLL may experience discomfort, swelling, and pain in the abdomen if their spleen enlarges. In rare cases, CLL can also affect mucosal tissues, such as those lining the gastrointestinal (GI) tract.
This article discusses the link between CLL and stomach pain in more detail. It also looks at ways to prevent and treat CLL, the other possible symptoms, and the outlook for people with this condition.
People with CLL may experience various symptoms involving the abdomen or stomach, such as:
- discomfort, pain, or tenderness
- feeling full after eating small amounts of food
- swelling
- diarrhea or vomiting
- abdominal cramping
- loss of appetite
- unexplained weight loss
In most cases, people with CLL do not experience abdominal symptoms due to the disease until it progresses and becomes more severe.
Research suggests that CLL infiltrates and affects the GI tract in about 5.7–13% of cases. When CLL affects the GI tract, doctors may call it Richter’s syndrome.
People with CLL may experience abdominal swelling, discomfort, and tenderness as a result of their spleen becoming larger. Less commonly, they may also feel full after eating small amounts of food, as the spleen can press on the stomach, making it smaller and able to hold less.
In rare cases, CLL infiltrates the lining of the GI tract, causing inflammation and ulcers or open wounds. People may experience symptoms similar to those of inflammatory bowel disease (IBD) and malabsorption disorders. These symptoms may include diarrhea, nausea, vomiting, abdominal pain and cramping, and unintentional weight loss.
CLL is cancer that develops in lymphocytes, which are white blood cells that form in the bone marrow and help fight infection.
Lymphocytes make up most of the lymph tissues in the lymph nodes, thymus gland, adenoids, tonsils, and spleen. They are also present in the GI tract, bone marrow, and respiratory system.
CLL is a type of leukemia that develops gradually over time.
About 50–75% of people with CLL do not experience noticeable symptoms. Due to this, doctors diagnose most people with CLL during routine blood work.
The symptoms of CLL often begin when the cancerous cells crowd out healthy cells in the bone marrow or migrate to other organs or tissues. When symptoms first appear, they are typically mild, but they then become increasingly severe. CLL can cause many nonspecific symptoms, so a person may feel as though they have a cold or the flu.
Possible symptoms of CLL that do not relate to the abdominal area include:
- swollen lymph nodes
- frequent infections that are difficult to recover from
- unexplained exhaustion or weakness
- unexplained breathlessness or breathing issues
- excessive or abnormal bruising
- nosebleeds and heavy periods
- bone pain
- night sweats
- low grade fever
- jaundice, which is a yellowing of the mucous membranes, whites of the eyes, or skin
Exploring Why Venetoclax and Ibrutinib Have Synergy in the CLL Population
Exploring Why Venetoclax and Ibrutinib Have Synergy in the CLL Population
This article was originally posted on Targeted Oncology
William G. Wierda, MD, PhD, D. B. Lane Cancer Research Distinguished Professor, section chief of Chronic Lymphocytic Leukemia, and center medical director in the Department of Leukemia, Division of Cancer Medicine, and executive medical director of The University of Texas MD Anderson Cancer Center, discusses the synergy between ibrutinib (Imbruvica) and venetoclax (Venclexta) in patients with chronic lymphocytic leukemia (CLL).
Ibrutinib, a Bruton’s Kinase inhibitor (BTK), inhibits a molecule that is downstream of the B-cell receptor–signaling pathway, BTK. It was approved for use in patients with relapsed disease first and then as frontline treatment in CLL. Wierda says it is very effective and active, including in patients who have been considered high-risk; these patients are defined as those who harbor 17p deletions or TP53 mutations.
Venetoclax is also a small molecule inhibitor that inhibits BCL-2. When patients’ CLL cells are exposed to venetoclax and BCL-2 is inhibited with this agent, it pushes the cells into apoptosis and causes cell death of the CLL.
Ibrutinib is very effective at managing this disease, according to Wierda. Clinically, it works well in shrinking lymph node size in these patients. Many of those who respond achieve a partial response. This means there is still some measurable disease, usually in the bone marrow or blood. Wierda says venetoclax is highly effective at killing CLL cells and is very potent at killing cells in the blood and bone marrow. However, it’s less active when it comes to shrinking nodal disease.
Higher Overall Response Rates Observed When Adding Ublituximab to Ibrutinib Treatment for CLL
Higher Overall Response Rates Observed When Adding Ublituximab to Ibrutinib Treatment for CLL
This article was originally published on CancerNetwork
The combination of ublituximab plus ibrutinib (Imbruvica) led to a statistically higher overall response rate while maintaining the tolerable safety profile over ibrutinib monotherapy to treat patients with relapsed or refractory high-risk chronic lymphocytic leukemia (CLL).
According to data published in The Lancet Haematology from the phase 3, multicenter, GENUINE (NCT02301156) trial, these findings support the addition of ublituximab to Bruton tyrosine kinase (BTK) inhibitors as treatment for patients with this class of CLL.
“Clinically meaningful improvements in overall response rate, complete response, and MRD negative response were observed and translated into improved progressionfree survival,” wrote the investigators. “These findings indicate the benefit of adding the nextgeneration antiCD20 antibody ublituximab to ibrutinib in patients with relapsed and refractory high-risk chronic lymphocytic leukaemia.”
The overall response rate was 83% of patients in the ublituximab plus ibrutinib group and 65% of patients in the ibrutinib group (P = .020) after a median follow-up of 41.6 months (IQR 36.7–47.3).
While the safety profile consisted mostly of grade 1 or 2 adverse events, neutropenia (19% of patients in the combination group vs 12% in the control group), anemia (8% vs 9%, respectively), and diarrhea (10% vs 5%) were common grade 3 and 4 adverse events among the population of interest.
More, common serious adverse events included pneumonia (10% with ublituximab vs 7% with ibrutinib only), atrial fibrillation (7% vs 2%, respectively), sepsis (7% vs 2%), and febrile neutropenia (5% vs 2%).
Two patients from the ublituximab plus ibrutinib group and 5 patients and from the ibrutinib group died from adverse events. Only 1 death (cardiac arrest) from the ibrutinib group was considered treatment-related.