ASH 2020 CLL Daily Wrap-Up
ASH 2020 CLL Daily Wrap-Up
This article was originally published on Patient Power
Overview
Join Patient Power on Tuesday, December 8th at 4pm PT/7pm ET for a live recap of the latest chronic lymphocytic leukemia (CLL) news from the 62nd American Society of Hematology (ASH) Annual Meeting. ASH is the world’s most comprehensive hematology event of the year where experts review thousands of scientific abstracts, highlighting updates on the most critical topics in hematology. Some of the field’s top doctors will share their thoughts on emerging research, clinical trials, and how current events such as COVID-19 are impacting cancer patients. Attend live to hear exciting CLL news from ASH 2020!
This program is sponsored by Pharmacyclics. This organization has no editorial control. It is produced by Patient Power. Patient Power is solely responsible for program content.
CLL and COVID-19: What Should Patients Know About Vaccines?
CLL and COVID-19: What Should Patients Know About Vaccines?
This article was originally published on Patient Power
What Vaccinations Should CLL Patients Receive?
With the flu season approaching and whispers of a vaccine for COVID-19 in the works, CLL patients with compromised immune systems may have questions about what vaccines they should be receiving, and if there are any risk factors involved. According to the experts, patients with CLL should schedule their flu shots right away, but what is recommended for a future COVID vaccine?
Listen in to find out more! Carol Preston, host and CLL patient advocate, will speak with Paolo Caimi, MD, Hematologist/Oncologist at University Hospital (UH) Cleveland Medical Center on these important topics.
In the Future, Should CLL Patients Get a Vaccine for COVID-19?
Carol Preston:
There is no vaccine at this time. We don’t know exactly when there will be a vaccine. And we know as CLL patients that we are only supposed to have dead vaccines as opposed to live viruses in a vaccine. So what is your thinking about a future COVID-19 vaccine.
Dr. Caimi:
What I am telling my patients is when the vaccine comes, we will first have to make sure that it’s safe. Second, I have to make sure that it’s safe for you. Meaning that for people with bad immune systems or people with half bad immune systems. Third, we’ll have to figure out with people who are less young, whether the dosing is different, whether the regimen is different. Then third, I’ll say probably what I’ll want them to do is to have everybody else around them vaccinated. Right?
So, in general, our patients are the ones who need to be beneficiaries of herd immunity, meaning everybody else’s immune to virus can’t touch them. And that’s probably what I would recommend them first to say, everybody else around you needs to be your barrier of protection for a vaccine. Once we figure out what the vaccine is going to be of benefit for you, maybe you need a different dosing, then we go ahead with it.
NICE recommends new chemo-free chronic lymphocytic leukaemia treatment
NICE recommends new chemo-free chronic lymphocytic leukaemia treatment
This article was originally published on EPR
The UK’s National Institute for Health and Care Excellence has recommended a new chemotherapy-free treatment for people with untreated chronic lymphocytic leukaemia (CLL). The institute said its recommendation of venetoclax plus obinutuzumab could benefit more than 1,000 people each year.
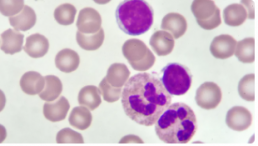
The innovative 12-month treatment will be offered to people with CLL who have not received any prior treatments. CLL affects white blood cells and is the most common chronic leukaemia, accounting for 30 percent of all adult leukaemias. In England there were 3,157 new cases of CLL in 2017.
Venetoclax plus obinutuzumab will be offered as a first-line treatment to people with CLL, with certain genetic abnormalities (such as a 17p deletion or TP53 mutation). For those without a 17p deletion or TP53 mutation, venetoclax plus obinutuzumab will be offered to patients with untreated CLL for whom fludarabine plus cyclophosphamide and rituximab (FCR) or bendamustine plus rituximab (BR) is unsuitable. The combination has also been made available via the UK’s Cancer Drugs Fund for this indication, so more evidence can be gathered on its cost effectiveness.
When and How CLL, SLL Should Be Treated
When and How CLL, SLL Should Be Treated
This article was originally published on Cure
Treatments for chronic lymphocytic leukemia (CLL) and small lymphocytic leukemia (SLL) have drastically improved in recent years, although patients may not need immediate treatment directly after being diagnosed.
Then, once it is decided that a patient will undergo treatment, deciding on the timing and regimen is pivotal.
When to Treat CLL/SLL
To determine if treatment is needed, patients should talk with their providers about symptoms they are experiencing, swollen lymph nodes, and blood cell counts, according to Dr. Locke J. Bryan, associate professor of medicine at the Medical College of Georgia and the hematology/oncology fellowship program director at the Georgia Cancer Center at Augusta University.
Bryan discussed CLL and SLL at the CURE® Educated Patient Leukemia & Lymphoma Summit.
One symptom of CLL and SLL is swollen lymph nodes; the location of the swelling could play a role in whether or not the disease is treated.
“It’s about location … a big node may not be causing any problems, but a smaller node pushing on an organ may cause some problems. Then, yes, the patient may need some treatment,” Bryan said. “And then as those (white blood cell) counts start to drop, that may be another reason.”
Dr. Awan on the Importance of Collaborative Care in CLL
Dr. Awan on the Importance of Collaborative Care in CLL
This article was originally published on Onc Live
The field of CLL continues to excel forward with novel molecular biomarkers, new therapeutic options, and ongoing clinical trials, says Awan.
Despite this, CLL remains a complex disease, Awan adds. As such, closely collaboration between community oncologists and CLL experts is often necessary to ensure patients receive optimal care.
Moreover, individuals who treat many cases of CLL may be able to recommend ongoing clinical trials that community oncologists are not aware of, Awan adds.
Ultimately, collaborative care is needed to identify new treatments and testing options, and to improve upon available therapies, Awan concludes.
Different Therapies and Modalities for Treatment of CLL in the Second Line
Different Therapies and Modalities for Treatment of CLL in the Second Line
This article was originally published on Targeted Oncology
During a Targeted Oncology Case Based Peer Perspectives event, Danielle Brander, MD, assistant professor of Medicine at Duke Cancer Institute in Durham, NC, discussed options for treating a 53-year-old female patients with chronic lymphocytic leukemia (CLL).
Targeted Oncology™: What are the guideline-recommended regimens to treat a patient with CLL such as this one?
BRANDER: The [National Comprehensive Cancer Network] guidelines for regimens in the relapsed/refractory setting include acalabrutinib [Calquence] and venetoclax [Venclexta], which are approved in all lines of therapy. In the relapsed/refractory setting, there’s also approval of duvelisib [Copiktra] and idelalisib [Zydelig], which are PI3K inhibitors.1
What data support the use of ibrutinib (Imbruvica), which is another guideline-recommended agent for the treatment of this patient?
The data that led to the initial approval of ibrutinib was the RESONATE trial [NCT01578707]. [The trial] randomized patients 1:1 to either ibrutinib or the anti-CD20 antibody standard-of-care agent in the relapsed/refractory setting, ofatumumab. Patients were allowed to cross over on this study.2
There are now 6-year follow-up data [showing that the] median progression-free survival [PFS] for the ibrutinib arm was not reached but was short [8.1 months] for the ofatumumab alone [HR, 0.133; 95% CI, 0.099-0.178].
Markers [of prognosis] that would indicate inferior response to chemoimmunotherapy are either the patients with IGHV unmutated or del(17p) or del(11q), who are still having good responses. This is in the relapsed/refractory setting with novel agents.
The grade 3 or greater AEs [adverse effects] that you’ll see are infectious complications. Infections and neutropenia do get better in terms of incidence with [time]. But obviously, if they have to stop [treatment] in the first year, it’s still detrimental to them. One thing [to keep in mind when] monitoring patients is that time on therapy does increase risks for hypertension. Atrial fibrillation and bleeding remain a risk throughout treatment. Often, they first appear early on treatment.
Dr. Davids on Factors to Inform Treatment Selection in CLL
Dr. Davids on Factors to Inform Treatment Selection in CLL
This article was originally published by OncLive
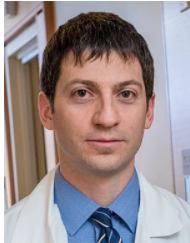
Matthew S. Davids, MD, MMSc, director of clinical research in the Lymphoma Program and a medical oncologist with Dana-Farber Cancer Institute, as well as an assistant professor of medicine at Harvard Medical School, discusses factors to consider when selecting treatment for patients with chronic lymphocytic leukemia (CLL).
When deciding which modality to select for patients with CLL, comorbidities must be considered, says Davids. For example, if there is a patient with significant cardiovascular disease, particularly if he/she is on an anticoagulation medication for atrial fibrillation, BTK inhibitors may not be the optimal choice. For this patient, a venetoclax (Venclexta)-based regimen should be considered, according to Davids.
On the other hand, if a patient has poor renal function and tumor lysis risk is a concern or if he/she is older and has difficulty commuting to the medical center for frequent monitoring, then a BTK inhibitor is favored, says Davids. With this approach, there is less risk of tumor lysis and patients require less monitoring than they would with a venetoclax-based regimen, concludes Davids.
The Role of Chemoimmunotherapy Dwindles Among New Regimens in Frontline CLL
The Role of Chemoimmunotherapy Dwindles Among New Regimens in Frontline CLL
This article was originally published by OncLive
Although frontline chemoimmunotherapy regimens have been the gold standard for patients with chronic lymphocytic leukemia (CLL) for many years, the advent of BTK inhibitors and other novel drugs has moved the field toward adopting chemotherapy-free options for patients in this setting.
“For 50 years or so, there weren’t too many major developments in this field,” said Matthew S. Davids, MD, MMSc, director of clinical research and the lymphoma program at Dana-Farber Cancer Institute. “We had some improvements in the intensity of chemoimmunotherapy regimens, but in the last 10 years, we have had some really remarkable developments where the whole field was transformed.”
In an virtual presentation during the 2nd Annual Precision Medicine Symposium, a program developed by Physicians’ Education Resource® LLC, Davids, who is also an associate professor of medicine at Harvard Medical School, discussed the switch to chemotherapy-free regimens and whether chemoimmunotherapy combinations will retain a role in the frontline treatment of patients with CLL.
Novel Therapies Challenge Standard Frontline Chemoimmunotherapy Regimens
Upfront fludarabine, cyclophosphamide, and rituximab (Rituxan; FCR) chemoimmunotherapy was considered the gold standard for patients with CLL. Moreover, studies such as the FCR 300 and CLL8 trials showed that time-limited FCR can provide functional cure in patients with IGHV-mutant CLL.1,2
“This does highlight the important role of IGHV mutation status when we are thinking about using chemoimmunotherapy,” explained Davids. “IGHV-unmutated patients tend to have steady disease progression over time and do not enjoy the potential functional cure [that IGHV-mutated patients may derive].”
Other chemoimmunotherapy regimens such as bendamustine and rituximab (BR), which is widely used in the community setting, according to Davids, and obinutuzumab (Gazyva) plus chlorambucil, are also active in the frontline CLL space.
However, in recent years, studies have demonstrated superiority with novel regimens compared with chemoimmunotherapy.
“Much of [the advancements made in CLL] are due to the investment in basic science that was done in the late 1990s and early 2000s that allowed us to understand the role of the microenvironment in CLL and how that can be leveraged to treat the disease,” said Davids.
For example, in the phase 3 ECOG 1912 trial, the combination of the BTK inhibitor ibrutinib (Imbruvica) and rituximab, followed by ibrutinib maintenance therapy, demonstrated favorable progression-free survival (PFS) compared with FCR chemoimmunotherapy in patients 70 years or younger with previously untreated CLL.3
At a median follow-up of 33.6 months, the PFS rate was 89.4% with the ibrutinib/rituximab regimen versus 72.9% with chemoimmunotherapy (HR, 0.35; 95% CI, 0.22-0.56; P < .001). Moreover, overall survival (OS) also favored the chemotherapy-free regimen at 98.8% versus 91.5% with chemoimmunotherapy (HR, 0.17; 95% CI, 0.05-0.54; P < .001).
However, at 3 years, the PFS rate in patients with IGHV-mutant disease was 87.7% with ibrutinib/rituximab versus 88% with FCR (HR, 0.44; 95% CI, 0.14-1.36).
Although these chemotherapy-free options have been revolutionary in the frontline treatment of patients with CLL, chemoimmunotherapy may still be considered in this particular subgroup of IGHV-mutant patients, according to Davids.
“For my young fit patients with IGHV-mutant disease, FCR is certainly still part of the conversation,” Davids explained, adding that data suggest BR and obinutuzumab/chlorambucil are also options for these patients. In particular, BR should be considered for older, frail, IGHV-mutant patients who have cardiovascular comorbidities since giving BTK inhibitor therapy could increase the risk of cardiovascular events.
Similarly, results from the randomized phase 3 ELEVATE-TN trial demonstrated that acalabrutinib (Calquence) with or without obinutuzumab significantly improved PFS over obinutuzumab/chlorambucil chemoimmunotherapy.4 The median PFS at 28.3 months of follow-up was not reached with acalabrutinib as monotherapy or in combination with obinutuzumab versus 22.6 months with chemoimmunotherapy (HR, 0.1; 95% CI, 0.06-0.17; P < .0001; HR 0.20; 95% CI, 0.13-0.30; P < .0001).
Moreover, Davids added, chemoimmunotherapy may be selected in patients who prefer a time-limited therapy versus continuous treatment with a newer regimen.
“We can give 6 months of FCR and know that we have a good chance of very long-term remission,” said Davids. “We do have to counsel patients about cytopenias, infection risk, and secondary myeloid neoplasms. [These] are slightly more common in patients with CLL treated with FCR, but the rates are low.”
CLL14 Trial Aims to Eliminate the Need for Chemotherapy Altogether
The extended follow-up from the phase 3 CLL14 trial showed that the estimated 24-month PFS rate was 88.2% with the combination of venetoclax (Venclexta) and obinutuzumab versus 64.1% with obinutuzumab/chlorambucil.5 Although there was no statistically significant difference in OS between arms, venetoclax/obinutuzumab was associated with a low incidence of high-grade adverse effects in patients with relevant comorbidities.
Triple Therapy for CLL Shows Promise in Phase 2 Trial
Triple Therapy for CLL Shows Promise in Phase 2 Trial
This article was originally published by Cancer Therapy Advisor
Results from a phase 2 study of 3 oral targeted agents for chronic lymphocytic leukemia (CLL) showed that patients achieved deep remissions after a limited-time duration treatment. The study, published in the Journal of Clinical Oncology, included both treatment-naive patients and those with recurrent/relapsed disease.1 The regimen worked well enough that phase 3 studies are underway.
Patients in this trial (ClinicalTrials.gov Identifier: NCT02427451) received a combination regimen of obinutuzumab, ibrutinib, and venetoclax.2 The 3 agents have different mechanisms of action, and are thought to combine well against CLL. Obinutuzumab, an anti-CD20 monoclonal antibody, is given first, followed by ibrutinib, which inhibits the B-cell signaling protein Bruton tyrosine kinase (BTK). Venetoclax, a BCL-2 inhibitor, comes last.
“We took the 3 most highly effective nonchemotherapy drugs that we had in CLL, put them in this regimen, and dosed them so they’re started sequentially,” said the study’s lead investigator Kerry Rogers, MD, hematologist with The Ohio State University Comprehensive Cancer Center’s Arthur G. James Cancer Hospital and Richard J. Solove Research Institute in Columbus.
Uncommon Mutation in CLL Associated With More Favorable Prognostic Factors
Uncommon Mutation in CLL Associated With More Favorable Prognostic Factors
This article was originally published by Cancer Therapy Advisor
Patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) who had an MYD88 L265P mutation were uncommon and had distinct features, reported a cohort study in Blood Cancer Journal.
Study researchers identified 56 (3.1%) patients with CLL/SLL who had MYD88 mutations among 1779 who underwent mutational analysis. The study also included 100 patients who did not have MYD88 mutations to serve as a control group.
Among patients with MYD88 mutations, 38 (68%) had the L265P mutation and 18 (32%) had non-L265P mutations, which included 10 with V217F and 4 with M232T. Among the remaining patients with non-L265P mutations, 2 had a single-nucleotide mutation, 1 with S219C and the other with A6fs, and 2 had concurrent mutations, 1 with N291S/T294P and the other with F252I/M232T.
No morphological differences were seen, as all patients had a typical CLL morphology. In general, patients with non-L265P mutations had similar features to patients with wild-type MYD88.