Uncommon Mutation in CLL Associated With More Favorable Prognostic Factors
Uncommon Mutation in CLL Associated With More Favorable Prognostic Factors
This article was originally published by Cancer Therapy Advisor
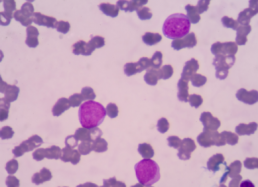
Patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) who had an MYD88 L265P mutation were uncommon and had distinct features, reported a cohort study in Blood Cancer Journal.
Study researchers identified 56 (3.1%) patients with CLL/SLL who had MYD88 mutations among 1779 who underwent mutational analysis. The study also included 100 patients who did not have MYD88 mutations to serve as a control group.
Among patients with MYD88 mutations, 38 (68%) had the L265P mutation and 18 (32%) had non-L265P mutations, which included 10 with V217F and 4 with M232T. Among the remaining patients with non-L265P mutations, 2 had a single-nucleotide mutation, 1 with S219C and the other with A6fs, and 2 had concurrent mutations, 1 with N291S/T294P and the other with F252I/M232T.
No morphological differences were seen, as all patients had a typical CLL morphology. In general, patients with non-L265P mutations had similar features to patients with wild-type MYD88.
Targeted Molecular Therapies for the Treatment of Chronic Lymphocytic Leukemia
Targeted Molecular Therapies for the Treatment of Chronic Lymphocytic Leukemia
This article was originally published by Hematology Advisor
Chronic lymphocytic leukemia (CLL) presents as an accumulation of monoclonal, mature, CD5+ B-cells in secondary lymphatic organs where cancer cells engage in molecular and cellular interactions disrupting the adaptive immune response. Promising advances in therapy options for patients with CLL, targeting these molecular interactions, were discussed in a review published in The New England Journal of Medicine.1
Since the introduction of these novel therapeutics, the use of chemoimmunotherapy has drastically declined. “We have moved away from using chemotherapy for most patients, just over the last 5 years”, Jan Burger, MD, PhD, of the department of leukemia at the University of Texas MD Anderson Cancer Center in Houston, told Hematology Advisor.
“We now have good alternatives to chemotherapy that, in the end, have better survival rates for our patients” Dr Burger, who is the author of the review paper, continued. “The reason why we were able to make this big step forward in treatment was to some extent [serendipitous]. These new kinase inhibitors became available at a time when there was more basic research which emphasized how important these molecules are in leukemia cells.”
Which Drug Therapy for CLL, Time-Limited or Continuous?
Which Drug Therapy for CLL, Time-Limited or Continuous?
This article was originally published by Medscape
About two thirds of patients who are diagnosed with chronic lymphocytic leukemia (CLL) are initially managed with a ‘watch-and-wait’ approach, but other one third of patients will need to be started on drug therapy straight away. But with which regimen?
The standard therapy to date has been time-limited chemoimmunotherapy, and this still has a key role to play in certain cases. But evolving continuous treatments and evidence on the array of factors that can influence response are making decision-making more individualized than ever, said Matthew S. Davids, MD, MMSc, director of clinical research in the Division of Lymphoma at Dana-Farber Cancer Institute and associate professor of medicine at Harvard Medical School, Boston, Massachusetts.
“Continuous versus time-limited treatment discussions are long discussions now and should be individualized to particular patients and their comorbidities,” said Davids.
Davids was speaking at a “How I Treat” session at the recent American Society of Hematology’s (ASH) Meeting on Hematological Malignancies, which was held virtually because of the COVID-19 pandemic.
Key Factors to Consider
Key factors in determining the most effective approach are the patient’s TP53 and immunoglobulin heavy chain (IGHV) gene mutation status, Davids said.
For instance, the traditional choice for frontline care for CLL has been standard chemoimmunotherapy (eg, fludarabine, cyclophosphamide and rituximab [FCR]), with a typical treatment duration of 6 months. However, the response effects appear most durable in younger patients with mutated IGHV and intact TP53.
As evidence, Davids cited data from a long-term follow-up of one of the original FCR studies in 300 patients, which found that about 60% of patients had long-term disease-free survival.
EU approves Imbruvica plus rituximab in first-line CLL
EU approves Imbruvica plus rituximab in first-line CLL
This article was originally published by The Pharma Letter
Johnson & Johnson (NYSE: JNJ) and AbbVie (NYSE: ABBV) have secured approval for a broader label for the BTK blocker Imbruvica (ibrutinib) in Europe.
The decision extends the approved indication in chronic lymphocytic leukemia (CLL) to include first-line treatment in combination with the targeted biologic therapy rituximab, and comes months after the US regulator provided approval in the same indication.
The decision is based on data from the Phase III E1912 study, which provides a favorable comparison with the established chemo-immunotherapy regimen fludarabine, cyclophosphamide and rituximab (FCR).
Profitable partnership
First approved in 2013, Chicago-based AbbVie (NYSE: ABBV) is jointly developing and commercializing Imbruvica with J&J’s pharma arm, Janssen.
The firms are in an equal partnership in developing the drug, after AbbVie acquired the original development partner Pharmacyclics for $21 billion in 2015.
The new approval in CLL represents the 11th approval overall for the product, and the sixth approval for Imbruvica in this cancer type.
Clinical Trials Survey 2020
Clinical Trials Survey 2020
Andrew Schorr, Patient Power co-founder, is the virtual keynote speaker to hundreds of people who supervise cancer clinical trials. The event is on September 10th. The event organizers want Andrew to share his perspective – and yours – on participation in cancer clinical trials now, during the time of the pandemic.
Please help Andrew give a powerful speech based on your experiences and thoughts around clinical trials in context of Covid-19.
The survey will just take a couple of minutes of your time. Thanks for helping and feel free to share with other patients!
Acalabrutinib Shows Promising Results for the Treatment of CLL
Acalabrutinib Shows Promising Results for the Treatment of CLL
This article was originally published by Targeted Oncology
Jennifer Woyach, MD, an associate professor in the Department of Internal Medicine at The Ohio State University Comprehensive Cancer Center–James, discusses the rationale and efficacy for the phase 1/2 trial of acalabrutinib (Calquence) in patients with chronic lymphocytic leukemia (CLL).
Woyach explains that acalabrutinib is an inhibitor of Bruton’s kinase (BTK), and it’s a second-generation covalent inhibitor. Similar to ibrutinib (Imbruvica), it binds irreversibly to BTK, but it is more selective than ibrutinib. Ibrutinib inhibits many structurally similar proteins, while acalabrutinib inhibits less, which is important for toxicity. She thinks that some of the toxicity seen with ibrutinib are because of those alternative targets. Some of the toxicities may lessen with acalabrutinib.
In treatment-naïve and relapsed/refractory disease, the data has looked promising with this agent, according to Woyach. In 1 study with 53 months of follow-up for 99 patients with treatment-naïve CLL, about 86% of the patients were still on treatment, which she says is impressive. The event-free survival at 48 months was 90%. This is looking promising with acalabrutinib, which is similar to what has been seen with ibrutinib in this patient population. Although she says it’s difficult to compare trial to trial, it’s good to see that it looks similar to ibrutinib in this setting.
Can Culturing CAR T Cells With Ibrutinib Improve Their Efficacy in CLL?
Can Culturing CAR T Cells With Ibrutinib Improve Their Efficacy in CLL?
This article was originally published by Cancer Therapy Advisor
Efficacy of chimeric antigen receptor (CAR) T-cell (CAR-T) therapies in chronic lymphocytic leukemia (CLL) have lagged behind the efficacy they appear to have in other hematological malignancies such as acute lymphoblastic leukemia or diffuse large B-cell lymphoma.
There’s a growing recognition that some of the CAR-T shortfalls in CLL are due to an impaired fitness of T cells in CLL patients. Some research has shown, however, that sustained remission of CLL is associated with enrichment of a less-differentiated, early-memory phenotype of T cells in the apheresis product used to make CAR-T therapies.1 Such findings have galvanized interest in approaches to enhance this T-cell population during the immunotherapy manufacturing process as a possible route for overcoming treatment resistance.
Now, a small study in the International Journal of Cancer reported that culturing CLL patients’ T cells with the tyrosine kinase inhibitor ibrutinib — which among other effects, inhibits a pathway involved in T-cell differentiation — boosted the viability, function, and expansion of CLL patient-derived CAR T cells as well as enriching them with a less-differentiated phenotype.2
“Medical Cannabis: Knowledge, Attitudes and Expectations amongst NZ Health Care Professionals and their Patients”
Invitation to take part in survey:
“Medical Cannabis: Knowledge, Attitudes and Expectations amongst NZ Health Care Professionals and their Patients”
Dr Karen Oldfield is a PhD candidate at the Victoria University of Wellington and a Senior Clinical Research Fellow at the Medical Research Institute of New Zealand who is looking at the use of cannabis as a cancer medicine in NZ. All information collected will be treated in a confidential manner and will not be disclosed to any other agencies. If you are interested in helping with this research, read on…
Dr Oldfield has approached CLL Advocates NZ to invite CLL patients to take part in this project:
“Medical cannabis is a topical subject. As part of my PhD research, I am seeking NZ residents over the age of 18 with an oncology/cancer diagnosis to take part in a 5-10 minute online survey about their thoughts about the use of cannabis as medicine. For further information, you can find the participant information sheet here https://is.gd/OncInfo2 . If you are keen to take part, please find the survey at the following link: https://is.gd/OncPatientQ. Thanks for taking the time to consider participating in this research!”
We encourage you to help with this valuable study.
CLL Diagnosis Preceded by Decades of Increased Infection Susceptibility
CLL Diagnosis Preceded by Decades of Increased Infection Susceptibility
This article was originally published by Cancer Therapy Advisor
Chronic lymphocytic leukemia (CLL) is well known for its close relationship with immune dysfunction, with around a third of patient deaths attributable to bacterial or viral infections. And while the relative risk of death due to the malignancy itself has declined over the past few decades, the risk of death from infection among those with CLL has remained constant, some research suggests.1
Infections often precede a formal diagnosis of CLL. Patients are known to suffer severe infections such as pneumonia up to 10 years prior to being diagnosed. Such findings pose a chicken-or-egg conundrum: Does the immune dysfunction occur prior to the development of CLL, potentially driving the development of the malignancy, or do CLL cells arise first, causing immune dysfunction long before the disease is diagnosed?
Shedding fresh light on this question, a group of Danish researchers undertook a retrospective analysis of nationwide Danish cancer registries and examined CLL patients’ history of antimicrobial use as a proxy for infection susceptibility. In line with previous studies, the researchers found that antimicrobial use began to rise 6 years prior to CLL diagnosis.
But even before then, patients with leukemia had used more macrolides, antimycotics, and antivirals than healthy controls for up to 22 years before they were diagnosed. The authors wrote that this time window jibes well with the theory that immune dysfunction, and/or infections, develop prior to CLL and could potentially play a causal role in driving the disease. The findings were published last month in Leukemia.2
Burger Reviews BTK Inhibitors and Beyond in Frontline CLL
Burger Reviews BTK Inhibitors and Beyond in Frontline CLL
This article was originally published by Targeted Oncology
During a virtual Case Based Peer Perspectives event, Jan A. Burger, MD, PhD, professor, Department of Leukemia, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center in Houston, TX, discussed testing and the treatment options for chronic lymphocytic leukemia (CLL), based on the a case of 71-year-old female patient.
Targeted OncologyTM: What testing would you order to confirm diagnosis if you saw this patient in the clinic?
BURGER: We need to establish the diagnosis by flow cytometry and then we would do, at a minimum, FISH cytogenetics and, ideally, the mutational status. Cytogenetics can change, but
mutational status usually doesn’t change. If that’s been established somewhere outside [of your clinic], then you don’t have to repeat that test.
It’s important to repeat cytogenetics if you talk about the relapse setting. But here, we’re treating in the frontline setting, and she was tested. She was found to be IGHV unmutated and [positive
for] del(11q). That, traditionally, has been regarded as a higher-risk disease status because these patients respond OK to standard chemotherapy, but they have short remissions and survival times with FCR [fludarabine, cyclophosphamide, and rituximab (Rituxan)], BR [bendamustine plus rituximab], and those kinds of regimens compared with low-risk patients, such as those [who are positive for] deletion 13q and have IGHV mutated disease.
In terms of these sequences, when you see a patient with lymphocytosis, you send for flow cytometry, and part of the flow cytometry panel can test for additional markers, CD38 and ZAP-70. We have it [at MD Anderson], but I’m not sure if there are any outside routine flow cytometry labs reporting CD38 positivity or negativity or ZAP-70. These markers used to be very popular 10
years or so ago when IGHV-mutation status was not so commonly done and was more complicated to get. Nowadays, there’s a shift with sending a sample directly for IGHV-mutation testing.