CLL Advocates NZ Newsletter Issue 2
CLL Advocates NZ Newsletter Issue 2
A number of you will be familiar with and regularly reading HealthUnlocked and Patient Power, two patient support and networking services (based in the UK and US respectively) that cover CLL in detail.
For those not yet in the habit, I can recommend both websites to CLL patients, and their families and supporters. You can access both through our website on our useful links page here, or go directly to Patient Power here and HealthUnlocked here. Access is free.
HealthUnlocked is published daily, with ten articles in each edition, that are mainly personal stories and discussion among people with CLL, and also occasional reviews of CLL-related clinical studies.
One such study, in the 20 July edition was on CLL and Covid 19. It provided an analysis of the assessment of 190 patients with CLL who had proven Covid 19 infection. Most presenting for analysis (79%) were in the “severe” category (requiring ICU admission and/or oxygen). This is likely to be related to their having had contact with a hospital. One third of these patients died of Covid 19. The severe group were older than the less severe group, so increasing age is a risk. There was a reduced rate of severe disease in those patients who had had treatment recently as opposed to those who had treatment remotely, or never.
Patient Power (PP) sends email updates to subscribers, generally weekly. Their CLL articles tend to have more of a scientific and medical focus. They also regularly post videos of interviews conducted by the PP CEO, Andrew Schorr, who is a long-term CLL survivor. He interviews well known clinicians on aspects of CLL, including the latest research and developments in the understanding and treatment of CLL. His wife, Esther, also writes regularly for PP.
An interesting recent PP article discussed CAR T-cell treatment, which is being trialled for CLL in research centres globally, including the Malaghan Institute in Wellington (Dr Rob Weinkove).
As an aside on CAR T-cell therapy, I recently enjoyed a book by NZ comedian David Downs on his experience with cancer (in his case, lymphoma). The book is entitled “A Mild Touch of the Cancer”. It is humorous and insightful on living with a serious health issue, and I commend it to you.
Finally, if you haven’t already seen it, check out our message on Facebook and on our website about our first CLL education event, to be held in Auckland, on Wednesday 14 October 2020. The event will be jointly hosted with Leukaemia & Blood Cancer. For those unable to be there in person, you’ll be able to join us via Zoom, to hear talks by and discussion with three of our country’s foremost CLL clinicians. As well as providing the latest information on CLL we hope to extend our reach and ability to support people living with CLL, and I warmly encourage you to help spread the word and attend the event with your family and supporters. More detail on the event including how to register will be circulated soon.
With best wishes
Neil Graham FRACP, FRCP
Executive Director
CLL Advocates NZ
Genetic Prognostic Factors in CLL Treated With Novel Compounds
Genetic Prognostic Factors in CLL Treated With Novel Compounds
This article was originally published by Cancer Therapy Advisor
Treatment with obinutuzumab plus venetoclax (VenG) was associated with improved outcomes compared with obinutuzumab plus chlorambucil (CGlb) among patients with chronic lymphocytic leukemia (CLL) and established unfavorable genetic factors, according to a study published in Blood.1
“Genetic parameters are established prognostic factors in chronic lymphocytic leukemia (CLL) treated with chemoimmunotherapy, but are less well studied with novel compounds,” the authors wrote.
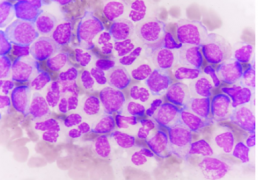
Unmutated IGHV, mutated TP53, and deletion of chromosome 17p (del[17p]) that contains the TP53 locus, are associated with progression and shorter survival among patients with CLL treated with chemoimmunotherapy. Other genetic markers have been identified that are also prognostic for outcomes.
This analysis used data from the multicenter, phase 3 CLL14 trial, which randomly assigned 432 patients with CLL to receive first-line VenG or CGlb. The analysis used fluorescence in situ hybridization (FISH), DNA sequencing, and next-generation sequencing to evaluate genetic prognostic factors.
CLL Experts Favor Social Distancing, but Vary on Treatment Continuation Amid Pandemic
CLL Experts Favor Social Distancing, but Vary on Treatment Continuation Amid Pandemic
This article was originally published by AJMC
The survey is the latest attempt to figure out how best to manage patients with CLL amid the pandemic, given that patients with the cancer tend to be older in age, have comorbidities, and be immunosuppressed.
In a letter to the editor of the American Journal of Hematology, corresponding author Mazyar Shadman, MD, MPH, of the Fred Hutchinson Cancer Research Center, in Seattle, and colleagues reported on a survey sent to 62 CLL specialists in the United States, Canada, Europe, and Australia. Of those, 59 responded to at least 1 question, and 44 completed the entire survey.
When asked about social distancing recommendations for patients with CLL, 32% said they would advise patients to follow the same guidelines as the WHO and Centers for Disease Control and Prevention (CDC) recommend for the general public. Twenty-one percent said they would advise patients to follow those guidelines but also limit regular outings by asking friends to pick up groceries or medications for them. Another 35% went even further, saying patients with CLL should avoid work, even if they are essential workers. The remaining 12% said they would recommend all of the above, plus wearing N95 masks and gloves outside of the house.
In terms of testing, most experts said it was not necessary to test all patients with CLL for COVID-19. Specifically, 62% of experts said they would limit testing to patients who call to and report symptoms, and another 9.5% said tests should be limited to patients who come in for an office visit and report symptoms.
Still, while clinicians generally had a low bar for what types of symptoms warranted testing. “Most favored testing patients with any levels of reported symptoms, even with limited testing availability,” Shadman and colleagues wrote. “With unlimited access, 23% recommended universal testing.”
Though their approaches to social distancing and testing were in line with recommendations for the general public, the experts expressed caution when it came to continuation of outpatient therapy. Only 14% said CLL therapy should be continued unconditionally. Most (60.5%) favored treatment discontinuation, and 25.5% said they favored continuation only based on the specific clinical situation.
However, when it came to bruton tyrosine kinase inhibitors (BTKis), such as ibrutinib (Imbruvica) and acalabrutinib (Calquence), the proportion of experts favoring unconditional treatment continuation was much higher, at 44%.
Shadman and colleagues said the more favorable responses concerning BTKi continuation may be due to concern about disease flares if treatment were stopped.
“Also, there is a theoretical benefit of BTKi’s in blunting the hyperinflammatory stage of COVID-19 disease by targeting macrophages and/or inhibiting pro-inflammatory cytokines,” they said.
Most experts (72%) recommended against the use of intravenous immune globulin (IVIG), though the authors noted that the survey was conducted in late March and early April, “before passive antibodies in the gammaglobulin pool would be expected.”
Shadman and colleagues said additional study is warranted to better understand the optimal approach to management of patients with CLL during the pandemic.
Dr. Davids on the Potential Utility of Frontline Ibrutinib/Umbralisib in CLL and MCL
Dr. Davids on the Potential Utility of Frontline Ibrutinib/Umbralisib in CLL and MCL
This article was originally published by OncLive
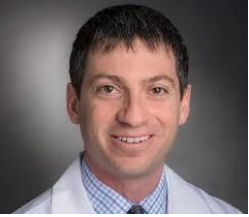
Matthew S. Davids, MD, MMSc, an associate director with the Center for Chronic Lymphocytic Leukemia; director of clinical research, Lymphoma Program; and medical oncologist, Dana-Farber Cancer Institute; and an assistant professor of medicine at Harvard Medical School, discusses the potential utility of moving the combination of ibrutinib (Imbruvica) and umbralisib into the frontline setting of chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL).
Findings from a phase 1/1b study presented during the 2020 European Hematology Association Annual Congress showed that ibrutinib/umbralisib elicited high response rates in CLL and MCL with a tolerable safety profile.
Updated data from the study revealed that progression-free survival and overall survival did not differ significantly from ibrutinib monotherapy in patients with MCL; however, outcomes were not negatively impacted.
In CLL specifically, the combination may have utility in the post-venetoclax (Venclexta) patient population as venetoclax is being used earlier in treatment, explains Davids.
Moving PI3K inhibitors into the frontline setting has been met with some challenges such as increased immune-mediated toxicities, says Davids.
As umbralisib appears to be a well-tolerated PI3K inhibitor, this combination may have potential utility in CLL, concludes Davids.
A 79-Year-Old Man With Relapsed Chronic Lymphocytic Leukemia
A 79-Year-Old Man With Relapsed Chronic Lymphocytic Leukemia
This article was originally published by Targeted Oncology
High-Risk Chronic Lymphocytic Leukemia
Jeff Sharman, MD: Hello, my name is Jeff Sharman. I’m the Medical Director of Hematology Research for US Oncology, and I am a practicing oncologist at the Willamette Valley Cancer in Eugene, Oregon.
Today I’ve been asked to present a case of a 79-year-old gentleman with relapsed chronic lymphocytic leukemia to address some of the treatment considerations we have in this patient population.
This particular patient is a hypothetical patient but referred to me. We’ll say that he was a 79-year-old gentleman who initially presented to his outside medical oncologist for the first time complaining of some vague intermittent abdominal pain and progressive fatigue. His past medical history is notable primarily for medically-controlled hypertension. He had a myocardial infarction 8 years ago and is on low-dose aspirin. His original CLL diagnosis was about 7 years ago, and after a period of watchful waiting, he had progressive lymphocytosis and adenopathy. He was treated with ibrutinib 420 mg daily, his symptoms improved, and he achieved a stable disease with resolution of lymphadenopathy.
Unfortunately, after 5 years of disease control on ibrutinib, he complained of increasing fatigue and decreasing appetite. Upon physical exam, he had a return of palpable lymphadenopathy, and his spleen was palpable, 4 centimeters below the costal margin. At that time, seen by an outside medical oncologist, he was started on rituximab monotherapy due to his medical comorbidities, but after 6 months on this regimen, he presents to my clinic after moving to be closer to family.
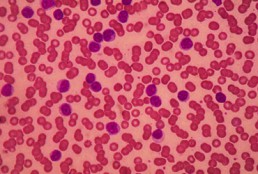
His physical exam was notable this time for palpable bilateral cervical adenopathy, right-sided inguinal adenopathy. Labs showed a white blood cell count of 55,000, predominately lymphocytes, and neutrophil count of 3100. He was anemic and thrombocytopenic, with a hemoglobin of 9.4 and platelets of 90,000, respectively. His beta-2 microglobulin was elevated, and, notably, he had a creatine clearance of just 31 mL per min.
Flow cytometry confirmed the typical immunophenotype for CLL, and at this time, FISH testing was performed and, importantly, returned a deletion of 17p in a high fraction of the cells. He was Rai stage 4 with an ECOG performance status of 1. At this time, treatment was initiated with idelalisib in combination with rituximab, or I should say idelalisib was added to rituximab at this time, 150 mg PO BID.
Now this is an interesting case, and it presents a number of features that are challenging in terms of how to pick therapy in this population with significant comorbidities. I’ve been asked to address questions pertaining to both his prior management, his current situation, and so forth.
The first question I’ve been asked is to describe my initial impression of the case and what the prognosis was for this patient. You know this is a patient who has high-risk CLL. He has relapsed after ibrutinib, and he has a deletion of 17p. What that means is that chemoimmunotherapy is not going to work for this individual, so you really don’t have that much in the way of options. Then you’ve exhausted BTK inhibitors, and there’s a question of what you have left.
In this particular case, the outside provider used rituximab monotherapy probably for lack of clarity in what options might have been available; this is a patient that because of his age and comorbidities, it’s very possible this patient may ultimately pass away of their CLL, which, in contemporary CLL management, seems like a relatively rare occurrence.
When we discuss risk stratification for patients with chronic lymphocytic leukemia, there’s a couple of things that are really important. We think about their IgHV status, which is really a measurement of how quickly the CLL is growing. What are the kinetics of growth? Then we think about the FISH status, which is how resistant it is to therapy. Deletion of 17p is a particularly noteworthy abnormality because patients with 17p have very brief responses to chemoimmunotherapy-based approaches.
Similarly, we’re seeing updates with targeted therapy, such as venetoclax, that 17p can retain adverse prognostic significance in this population. In this particular patient’s case, idelalisib had been added to the regimen. It’s noteworthy that idelalisib outcomes appear to be independent of 17p, so whether 17p is present or not, the outcomes relative to 17p don’t matter quite as much.
Transcript edited for clarity.
Case: A 79-Year-Old Man With Relapsed Chronic Lymphocytic Leukemia
Initial presentation
- A 79-year-old man presented to a new medical oncologist for the first time complaining of vague intermitted abdominal pain, and progressive fatigue
- PMH:
- Hypertension, medically controlled
- MI, 8 years ago, on 81 mg aspirin
- CLL, diagnosed 7 years ago
- After a period of watchful waiting he began treatment with ibrutinib 420 mg PO qDay; symptoms improved and achieved stable disease, resolution of lymphadenopathy
- After 5 years of disease control on ibrutinib he complained of increasing fatigue and decreased appetite, on physical exam there was return of palpable lymphadenopathy; spleen was palpable ~4 cm below costal margin
- He was started on rituximab
- Currently after 6 months on rituximab monotherapy he presents to the clinic
- PE: palpable bilateral cervical and right-sided inguinal lymphadenopathy
Clinical workup
- Labs: WBC 55,000, lymphocyte 82%, ANC 3100/mm3, Hb 9.4 g/dL, plt 90 x 109/L, LDH 220 U/L, Beta-2-microglobulin 3.9 mg/L; creatinine clearance 31 mL/min
- FC CD 5+, CD19+, CD20+ monoclonal B-cell population
- FISH: CLL probe set tested, deletion 17p
- IgHV mutational status: unmutated
- Rai stage IV; ECOG PS 1
- Treatment of idelalisib 150 mg PO BID was added to rituximab
Age, Recent Treatment, Appear to Influence Severity of COVID-19 in Patients With CLL
Age, Recent Treatment Appear to Influence Severity of COVID-19 in Patients With CLL
This article was originally published by AJMC
Patients with chronic lymphocytic leukemia (CLL) who contract coronavirus disease 2019 (COVID-19) face more severe symptoms if they are older, though recent treatment with antileukemic agents appears to have a beneficial, rather than detrimental, effect on outcomes, a new study found. The study also suggests that the presence of comorbidities does not lead to higher mortality rates.
The retrospective analysis is based on 190 patients with CLL who had confirmed COVID-19 cases between late March and late May. The results were published in the journal Leukemia.
Corresponding author Kostas Stamatopoulos, MD, PhD, of the Center for Research and Technology Hellas, in Greece, wrote along with colleagues that CLL is a “paradigmatic example” of a malignancy that has been associated with impaired immune responses to pathogens, which they said could have negative impacts on outcomes when patients with CLL contract COVID-19. The investigators added that antileukemic treatments could further hamper the immune system’s ability to fight off a virus like SARS-CoV-2, though they said it’s not a straightforward proposition.
“On the other hand, the severity of COVID-19 and [multiorgan failure] occurrence seem to be related to clinical and laboratory parameters of inflammatory response (lymphopenia, hypoalbuminemia, higher levels of alanine aminotransferase, lactate dehydrogenase, C-reactive protein, ferritin, and D-dimer) and markedly higher levels of proinflammatory cytokines (interleukin-2 receptor, IL6, IL-10, and tumor necrosis factor-α),” they said. “On these grounds, therapies targeting inflammation (eg, IL6/IL6R antibodies or steroids) have been used and shown potential benefit in full-blown COVID-19 patients.”
In an effort to ascertain a real-world understanding of what patients with CLL who contract the virus should expect, Stamatopoulos and colleagues analyzed the 190 colleagues based on age, gender, and comorbidities; severity of COVID-19; and whether and how long ago they had been treated with antileukemic therapies.
The investigators found a strong majority (151, or 79%) of patients presented with severe symptoms, such as requiring oxygen or admission to an intensive care unit. Patients were more likely to have severe symptoms if they were aged 65 or older.
Recent treatment appeared to make a significant difference. Only 4 in 10 patients with severe symptoms had received antileukemic treatment within the past 12 months. However, among those with mild symptoms, 76.9% had undergone recent treatment. Among those with severe symptoms, the likelihood of hospitalization was lower if they had received therapy with ibrutinib (Imbruvica).
More than one-third (36.4%) of patients with severe symptoms died from COVID-19; versus just 1 of the 38 patients with mild symptoms succumbed.
Stamatopoulos and colleagues noted that the apparent link between age and mortality among patients with CLL tracks with known data from the general population. However, they said comorbidities did not appear to have a significant impact on whether a patient had mild or severe symptoms.
As for the impact of antileukemic therapies, the authors said a disproportionate percentage of their study population had been prescribed bruton kinase inhibitors. Thus, they did not have sufficient data to compare the impact of BTK inhibitors to other types of therapy.
Still, they said their data seems to support the idea that recent antileukemic therapy is beneficial against COVD-19.
“Altogether, these data seem to further underscore the possible protective role of specific targeted therapies against a dismal evolution of the SARS-CoV-2 infection,” they said.
Dr. Ghia on the Shift From Chemotherapy to Novel Agents in CLL
Dr. Ghia on the Shift From Chemotherapy to Novel Agents in CLL
This article was originally published by Onc Live
Paolo Ghia, MD, PhD, a professor of Medical Oncology and the director of the Strategic Research Program on CLL and the B Cell Neoplasia Unit at Vita-Salute San Raffaele University, discusses how use the of chemotherapy is decreasing in favor of novel agents in chronic lymphocytic leukemia (CLL).
Chemotherapy regimens and chemoimmunotherapy treatment approaches are fading out of the treatment algorithm of CLL, says Ghia. This shift will be seen in the updated ASCO guidelines, where chemoimmunotherapy only remains an option for patients who do not have access to the novel therapies that are currently available in some countries and regions.
Not everyone has the same accessibility, but for the patients who do, particularly in the first-line setting, most of them experience a benefit from novel therapies. Even in the relapsed/refractory setting, the percentage of patients who benefit from chemoimmunotherapy is reducing with time, concludes Ghia.
Tool appears to predict need for treatment in asymptomatic, early-stage CLL
Tool appears to predict need for treatment in asymptomatic, early-stage CLL
This article was originally published by Healio
A novel prognostic tool appeared to predict the need for treatment among patients with asymptomatic, early-stage, chronic lymphocytic leukemia, according to research published in Blood.
“CLL is an indolent disease that is treated only if symptomatic. Currently, between 70% and 80% of newly diagnosed [patients with CLL] are asymptomatic and therefore are offered a wait-and-see approach to management consisting of regular visits every 3 to 12 months. However, this approach is not easily accepted by patients, who often ask whether, when and how they will be treated,” Davide Rossi, MD, researcher at Oncology Institute of Southern Switzerland, told Healio. “So far, the eventual disease course cannot be predicted for patients after they have been offered wait and see, which in turn causes anxiety and uncertainty. Having a tool that accurately forecasts leukemia course will help patients in planning their life with the disease.”
Rossi and colleagues developed and tested the international prognostic score, IPS-E, to predict time to first treatment among 4,933 patients with early-stage, asymptomatic CLL included in 11 global cohort studies.
Among a training cohort of 333 patients, investigators observed three consistent and independent covariates that appeared associated with time to first treatment: unmutated IGHV genes, absolute lymphocyte count greater than 15 x 109/l and the presence of palpable lymph nodes. They used data from this cohort to develop a prognostic score with each factor counting as one point. Patients with zero factors were considered at low risk for requiring treatment within the first 5 years of diagnosis, those with one factor were considered at intermediate risk, and those with two or three factors were considered at high risk.
Investigators validated the score in nine cohorts staged by the Binet system and in one study staged by the Rai system. They observed C-index scores of 0.74 in the training series and 0.7 in the aggregate of validation series.
Overall, approximately 30% of patients were categorized as low risk, 35% as intermediate risk and 35% at high risk.
Moreover, meta-analysis of the cohorts showed 5-year cumulative risk for treatment initiation of 8.4% among patients considered low risk, 28.4% for those in the intermediate-risk group and 61.2% for those at high risk.

“In a time where the treatment paradigm of asymptomatic CLL may change if a survival benefit is proven by early intervention with novel agents, our international prognostic score could help in defining the early-stage population where treatment can be appropriate,” Rossi said. “Moreover, it could be helpful for the treating physician to better allocate medical resources, such as deciding on the interval between clinical assessments according to risk group. Health care professionals will be supported in the discussion while explaining CLL to patients — many of whom have never heard about the rare tumor. Physicians can also safely plan and advise in advance the proper timing of surveillance visits according to the predicted risk of leukemia progression.”
The international prognostic score warrants prospective evaluation, according to Rossi, and can be regarded as a building block on which newly discovered independent outcome predictors for patients with early-stage CLL could be added.
“In this sense, a prospective study could be designed to further assess and eventually strengthen this prognostic tool,” Rossi said.
For more information:
Davide Rossi, MD, can be reached at Oncology Institute of Southern Switzerland, Via Ospedale, 6500 Bellinzona, Switzerland; email: davide.rossi@eoc.ch.
CLL and MCL Survival Benefit From Umbralisib Plus Ibrutinib Holds Up in 4-Year Follow-Up
CLL and MCL Survival Benefit From Umbralisib Plus Ibrutinib Holds Up in 4-Year Follow-Up
This article was originally published by Targeted Oncology
Initial results for the combination of umbralisib plus ibrutinib (Imbruvica) showed high rates of response in early 2019, but longer-term follow-up presented during the 2020 European Hematology Association (EHA) Congress demonstrated that complete responses increased over time in patients with relapsed/refractory chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL).
For patients with MCL, the median progression-free survival (PFS) was around 11 months, and the overall survival (OS) was around 2.5 years, which is not much different than what has been observed with ibrutinib monotherapy. However, in the CLL cohort, the 4-year PFS rate was 80%, and the 4-year OS rate was 90%, which was a big difference compared with historical controls.
Many patients are still receiving treatment with ibrutinib and umbralisib on the study, but this dataset highlights the continued efficacy and safety of dual B-cell receptor blockade. Umbralisib remains an investigational agent at this time, but more positive findings for this agent were recently presented from the phase 3 UNITY-CLL trial, which evaluated umbralisib in combination with ublituximab (TGTX-1101) in patients with CLL.
In an interview with Targeted Oncology, Matthew Davids, MD, MMSc, an associate director with the Center for Chronic Lymphocytic Leukemia; director of clinical research, Lymphoma Program; and medical oncologist, Dana-Farber Cancer Institute and an assistant professor of medicine with Harvard Medical School, discussed the long-term follow-up results of ibrutinib in combination with umbralisib as treatment of patients with CLL and MCL.
TARGETED ONCOLOGY: For patients with CLL and MCL, could you discuss the prognosis we see in this relapsed/refractory patient population?
Davids: With the advent of the BTK inhibitor ibrutinib, the outlook for patients with relapsed/refractory CLL and MCL certainly improved quite a bit. The drug is very active, and yet, particularly for high-risk patients and for CLL that means, especially patients with TP53 dysfunction, the durability of these responses is usually relatively short, so in that CLL high-risk population, looking at median PFS of only about 2 to 3 years in the relapsed setting with ibrutinib as a monotherapy. In MCL, even though the response rates are high, actually, the PFS is only a little over one year with a bruit nib as a monotherapy. That provided a rationale to try to develop combination approaches for this population, and there’s a number of them that are being evaluated right now.
The 1 combination that we focused on was looking at dual blockade of the B-cell receptor pathway. We know that the CLL cells and MCL cells depend heavily on this B-cell receptor pathway for survival and that there’s actually another arm of the pathway that has Pi3K as a key node. We were really interested in going after this other arm of the pathway to see if we could try to prevent resistance to ibrutinib as a monotherapy agent. That was the rationale for the study design.
TARGETED ONCOLOGY: What were the methods of design used for this study, and what did the patient population look like?
Davids: One of the challenges with this study is that there was a previous study that combined a SICK inhibitor drug with a Pi3K inhibitor and showed significant toxicity. That was the first time that there was a dual targeting of the B-cell receptor pathway, so we decided to take a different approach and rather than targeting SICK to target BTK, and rather than using an older delta-specific inhibitor of Pi3K, we used a newer molecule called umbralisib, which is a selective Pi3K inhibitor. It also targets casein kinase 2.
The idea here was to use 2 very well-tolerated drugs to target these 2 different parts of the pathway and try to prove that this could be a safe and effective strategy. We were able to accrue 42 patients to the study, 21 with CLL and 21 with MCL. These were all relapsed/refractory patients, generally with at least 1 to 2 lines of prior therapy. Few of them had had prior ibrutinib as mono therapy, but they weren’t refractory to ibrutinib; they had maybe started it but were still in the first few months of treatment. It was a pretty high-risk population as well, about 70% of the CLL patients had the unmutated IGhV and about 20% of the CLL patients had deletion 17p or TP53 mutation. This is generally quite a high-risk population. Many of the MCL patients had also relapsed already after autologous stem cell transplantation and were in desperate need of effective treatment options.
TARGETED ONCOLOGY: What were the results from this study?
Davids: We had published the initial results of this study early last year with around 2 years of follow up, and we did find the high rates of response in both CLL and MCL. We saw very good tolerability. We were able to identify the recommended phase 2 dose of umbralisib drug as 800 mg in combination with standard dose ibrutinib. The challenge with that early report was that the follow up was quite short, and so really the idea with our update at the EHA meeting is now with around closer to 4 years of follow up, looking at the progression-free and open overall survival for these very high-risk patients.
The other thing that we looked at actually was the rates of complete remission, which did increase a bit over time as we’ve seen with B-cell receptor pathway inhibitors. That was the case in our study as well. What we thought were the key updates from this poster were the PFS and OS data. Now with MCL, these didn’t change too much. The median PFS was only around 11 months in this very high-risk population, although the median OS was about 2 and a half years. To us, this didn’t look too different from ibrutinib a monotherapy, so it was hard to know if there’s a difference there. Where we are really seeing a difference is with the CLL patients. Obviously, we’re comparing to historical controls. There’s no there’s no randomized comparator here, but we did see a 4-year PFS in this high-risk CLL population of close to 80% and a 4-year OS of 90% in the CLL population with many patients still on the to drug combination, doing very well. Our data set here really highlights both the efficacy and the safety of dual B-cell receptor blockade, and I think this really does warrant further study.
TARGETED ONCOLOGY: Now that we’ve seen these promising results in the relapsed/refractory setting, is their evidence you think just for moving this up in the treatment landscape or in another patient population?
Davids: I think 1 patient population where this could be a useful approach is in the post-venetoclax (Venclexta) setting. Particularly in CLL, now we’re using venetoclax in earlier lines of therapy, including in the frontline setting. This type of approach might be very useful to use, for example, in the second-line setting; I think that needs to be explored. I think there have been challenges with moving other Pi3K inhibitor drugs into the frontline setting. We’ve seen more immune-mediated toxicities in those studies, but I do think with umbralisib being a very well-tolerated Pi3K inhibitor drug and ibrutinib being such a popular regimen for frontline CLL, certainly this type of approach could be studied in the frontline setting prospectively.
TARGETED ONCOLOGY: How do you see this combination potentially impacting the treatment landscape for CLL and MCL?
Davids: As of right now, umbralisib remains an investigational agent, although we did recently hear a press release about a positive result in the CLL UNITY study. I think that this is a drug that’s headed toward a label in CLL and possibly in MCL as well. Although right now, this is not a regimen that could be utilized, I do think it’s potentially a regimen that could be utilized off label in the future for a select group of patients. However, I would feel more comfortable as there’s more data accumulating in larger datasets to make this as more of a recommendation for patients. I think we need larger studies and ideally, a randomized study where we can compare a doublet like this to perhaps singlet therapy with ibrutinib.
Nonetheless, I think our study is the first time that we’ve shown the feasibility of combining a BTK inhibitor with a Pi3K inhibitor. We showed it in these 2 non-Hodgkin lymphomas, but I think this is the type of approach that could also be studied in other non-Hodgkin lymphomas and may be promising there as well.
Long-Term Results of Ibrutinib/Umbralisib Show Efficacy in CLL and MCL
Long-Term Results of Ibrutinib/Umbralisib Show Efficacy in CLL and MCL
This article was originally published by Targeted Oncology
Matthew S. Davids, MD, associate director of the Center for Chronic Lymphocytic Leukemia, director, Clinical Research for the Lymphoma Program at the Dana-Farber Cancer Institute, and associate professor of Medicine at Harvard Medical School, discusses the long-term follow-up of a phase 1/1b trial (NCT02268851) for patients with relapsed/refractory chronic lymphocytic leukemia (CLL) or mantle cell lymphoma (MCL) receiving ibrutinib (Imbruvica) and umbralisib.
The initial results were presented early in 2019 with about 2 years of follow-up, showing high rates of response in patients with CLL and MCL, according to Davids. There was good tolerability observed for these patients, and the investigators were able to identify the recommended phase 2 dose for umbralisib of 800 mg combined with the standard dose of ibrutinib.
The challenge with the initial report was that the follow-up for these patients was short, Davids says. The goal of the update at the 2020 European Hematology Association Congress was to present about 4 years of follow-up of the progression-free survival (PFS) and overall survival (OS) of the high-risk patients. The investigators also looked at the rates of complete remission, which increased over time.
For patients with MCL, the median PFS was around 11 months, and the median OS was about 2 and a half years. Davids thinks that this didn’t look much different than ibrutinib monotherapy, and it is hard to tell if there is a difference between monotherapy and this combination.
Davids says the investigators saw the bigger difference in the patients with CLL compared to historical control studies. There was about an 80% 4-year PFS in the high-risk CLL population and a 4-year OS of 90%. There are still many patients on the ibrutinib and umbralisib combination. The data set highlights the efficacy and safety of dual B-cell receptor blockade and warrants further study, he believes.