World Leukemia Day - 4 September 2020
World Leukemia Day - 4 September 2020
World Leukemia Day is on September 4th and we’d love you to join us.
We are looking for people from all around the globe to participate in increasing the awareness of leukemia that is so vital to help improve the lives of patients after diagnosis.
Here are 3 ways to get involved:
1. Share your leukemia story
Encourage others to share their leukemia story on social media and use the hashtags #WLD2020 or #WorldLeukemiaDay. More information is available at www.worldleukemiaday.org
2. Share your ‘spotty selfie’
Dig out your spotty clothes and share your ‘spotty selfie’ on social media with the hashtag #WLD20 on September 4th to show your support.
3. Spread the word
Help raise awareness of the symptoms of leukemia by using our social media graphics and sharing these across your social media platforms along with the hashtags #WLD20 #worldleukemiaday.
You can download all the social media graphics here > https://bit.ly/WorldLeukemiaDay
World Leukemia Day isn’t just about raising awareness, it’s also about education and learning how to spot the signs and symptoms. For some types of leukemia early diagnosis is crucial, if you are experiencing any of the symptoms, speak to a healthcare professional about your concerns.
Find out more about the signs and symptoms here > https://www.worldleukemiaday.org/what-is-leukemia
We look forward to seeing your ‘spotty selfies’ on September 4th.
Your CLL Advocates Network



CLL Advocates NZ Newsletter Issue 3
CLL Advocates NZ Newsletter Issue 3
Greetings
Research is a critical part of understanding diseases and their treatment. As set out in our Trust Deed, a key objective for CLL Advocates NZ is to ‘promote and support NZ-based research on CLL, including the value and importance of developing and participating in clinical trials, and improving the quality of NZ data on CLL. In pursuit of this objective we’re developing or supporting a number of initiatives:
- Clinical trials in NZ. You can find information on our website about ClinTrial Refer New Zealand. If you’re interested in keeping up to date with trials of CLL treatments in NZ, you can download the free app supported by HSANZ (Haematology Society of Australia and NZ) here. A number of New Zealanders have been enrolled in trials, often gaining access to unfunded medications, including “last resort” treatment options for advanced disease. There are numerous such trials actively recruiting as I write. One is Rob Weinkove’s work at the Malaghan Institute in Wellington, on CAR – T cell therapy. Trials of Zanubrutinib vs Ibrutinib are also recruiting in New Zealand.
- Second malignancies in CLL. We have proposed a summer studentship/research grant in the Bay of Plenty on this topic. Second malignancies are one of the commonest causes of death in CLL. They include Richter’s Syndrome and skin cancers, including melanoma. The project should start at the end of 2020. Having been a researcher in such studies myself, I know that patient involvement in research projects often significantly increases their own understanding of the disease, as they often involve frequent contact with health professionals and present good opportunities to talk about CLL with them.
- A PhD research study on the use of cannabis as a medicine for cancer patients. Dr Karen Oldfield is a PhD candidate at Victoria University of Wellington and a Senior Clinical Research Fellow at the Medical Research Institute of New Zealand, who is looking at the use of cannabis as a medicine in NZ. She’s inviting cancer patients to take part in a 5-10 minute online survey about their thoughts on this topic. All information collected will be treated as confidential. This is a valuable research project, as well as a way of fostering links between CLL patients and NZ research groups, and I warmly encourage you to take part. If you’re interested in helping with this research, go to this link on our website.
Finally, do remember the CLL forum we are having online and live at LBC headquarters on 14 October, 5.30 – 7.00pm. Invitations and details will be coming out shortly.
Best wishes
Neil Graham
Online webinar: Aggressive CLL Treatment Options: Are They Right for Me?
Online webinar: Aggressive CLL Treatment Options: Are They Right for Me?
How do experts decide when a CLL patient needs more aggressive treatments? In the age of oral therapy, when do CLL treatments such as CAR-T therapy and clinical trials make sense? Join us on Thursday, August 27th at 1 pm PT/4 pm ET for a live CLL Answers Now Program. Host Andrew Schorr will talk with University of Rochester Wilmot Cancer Center’s Dr. Paul Barr on these more aggressive treatment options for CLL. Please send questions in advance to cll@patientpower.info.
Thursday, August 27, 2020 at 1:00 PM Pacific Time (US and Canada)
CLLANZ will publish the link after the event has ended or you can register here
Understanding Chronic Lymphocytic Leukemia
Understanding Chronic Lymphocytic Leukemia
This article was originally published by Cure
Episode 3
Living with CLL as a Chronic Disease
Transcript:
Kristie L. Kahl: Should patients be getting retested if or when their disease recurs?
Dr. Susan O’Brien: There are some tests that we should be repeating anytime we’re considering a new treatment, that includes the FISH test which looks at chromosomal abnormalities inside the CLL cell as well as an important protein abnormality called the p53 mutation. A p53 mutation is a gene that can be mutated and the reason it’s super important to know about these chromosomes and the p53 status is that those patients should never receive chemo or chemo-immunotherapy because they don’t respond very well to it. But even with the small molecule therapies that we have nowadays, patients with those abnormalities can do better on one drug than another. So in other words, it’s important to know that because it may affect the physician’s choice of treatment.
Kristie L. Kahl: Outside of testing, are there other factors that should be considered when it comes to determining the next line of treatment?
Dr. Susan O’Brien: When you have treatment options, which we do nowadays, you want to look at the side effect profile. If you have a patient who has a history of atrial fibrillation or an irregular heart rate…maybe in that patient you want to go towards one of the other drugs. (Venclexta [venetoclax]) can cause tumor lysis so someone with a high-volume disease maybe you would be a little bit more cautious about using that. So you want to look at the side effect profile.
The other thing that’s important is that for some of these small molecules, the length of time that the patient is on the drug is different. So what do I mean by that? With (Imbruvica [ibrutinib]) or (Calquence [acalabrutinib]), the drug is given indefinitely. So once the patient starts on it they just continue on it unless they have a side effect which makes them stop or unless x number of years later the disease starts to come back and is then resistant to the drug. With venetoclax-based therapy, the regimen that’s approved for relapse is venetoclax with the antibody (Rituxan [rituximab]) and that’s a time limited therapy. So the rituximab is given for the first six months only and then the venetoclax is given daily for two years. So that treatment actually stops at two years and that may or may not be important to the patient if they have a time-limited therapy and that may or may not be important to the patient in terms of whether continuous therapy is a problem or time limit is more attractive.
We all know that in the states with oral agents there are copays and so in some senses having a limited time duration might be attractive. On the other hand, there are some patients who say well wait a minute if I’m responding to the drug you’re going to stop it anyway and they don’t like that idea so they actually would prefer to have an indefinite therapy as long as they’re tolerating it and it’s working.
So, I think you have to look at the side effect profiles of the drugs, that they’re different durations of time and then what the patient preferences might be or what’s most important to them.
Ibrutinib May Improve CAR T-Cell Production for Patients With Chronic Lymphocytic Leukemia
Ibrutinib May Improve CAR T-Cell Production for Patients With Chronic Lymphocytic Leukemia
This article was originally published by Targeted Oncology
Ibrutinib (Imbruvica) during chimeric antigen receptor (CAR) T-cell culture improved the yield and function of CAR T-cell products as treatment of patients with chronic lymphocytic leukemia (CLL) in a study published in the International Journal of Cancer.
The study investigators led by Leapold Sellner, MD wrote, “our study provides evidence that BTK/ITK inhibition with ibrutinib during CAR T-cell generation may improve CLL patient-derived CAR T cell products and may have the potential to enhance CAR T-cell function. Ibrutinib-supplemented CAR T-cell production leads to increased CAR T-cell yields as well as enriches for less-differentiated T cells with lower expression of exhaustion markers and could be an option to further improve the clinical outcome of CLL patients.”
Sellner et al evaluated the absolute cell numbers during CAR T-cell generation by Trypan blue staining. During cell generation, cell proliferation was significantly lower in CLL-derived cells compared with HD-derived cells. The BTK inhibitor allowed for a significant increase in cell expansion of HD-derived cells on day 10 of the CAR T-cell generation (20.67 ± 8.82 × 106 without ibrutinib vs. 25.28 ± 10.29 × 106 with ibrutinib; P =.0248), and ibrutinib appeared to significantly increase the viability of CD3-positive T cells from HDs on day 10 (3% ±8% vs 87% ± 7%; P =.0183) and day 14 (84% ± 8% vs 91% ± 6%, respectively; P =.0202).
TML Helps Predict Time to Treatment in CLL and its Precursor, Study Shows
TML Helps Predict Time to Treatment in CLL and its Precursor, Study Shows
This article was originally published by AJMC
Tumor mutational load (TML) can be used as a prognostic indicator in patients with chronic lymphocytic leukemia (CLL) and high-count monoclonal B-cell lymphocytosis (HC MBL), according to a new study.
The findings suggest that performing a focused mutation panel on recurrently mutated CLL genes could help risk-stratify patients and more accurately predict time to treatment (TTT).
Most patients who are newly diagnosed with CLL do not require therapy for a number of years, but some patients will require therapy right away. CLL’s precursor, HC MBL, will progress to CLL at a rate of 1-5% per year, but it can be difficult to predict how soon an individual patient will progress.
In hopes of better predicting patient progression, investigators from the Mayo Clinic conducted a study to analyze the total number of recurrently mutated CLL genes (TML) and the individually mutated genes beyond the CLL international prognostic index (CLL-IPI) in newly diagnosed patients with CLL and HC MBL.
To do so, they recruited 557 patients, 445 of whom had CLL and the remainder of whom had HC MBL, and sequenced 59 genes in the patients. Their goal was to identify links with TTT, adjusted for CLL and sex.
The authors found that TML correlated with shorter TTT. Among patients with low/intermediate risk, the link was even stronger when patients were stratified by CLL-IPI. Their results are published in the American Journal of Hematology.
Ball Score Predicts Benefit From Ibrutinib in CLL
Ball Score Predicts Benefit From Ibrutinib in CLL
This article was originally published by MedScape
The BALL score was able to identify a subset of patients with chronic lymphocytic leukemia (CLL) who particularly benefit from single-agent ibrutinib therapy, according to the results of a study of 111 patients followed from two different institutions.
The BALL model consists of four factors: serum beta₂-microglobulin at 5 mg/dL or greater, hemoglobin < 110 g/L for women or < 120 g/L for men, lactate dehydrogenase [LDH] > upper limit of normal [UNL], and time elapsed from last therapy less than 24 months. Each parameter was alloted 1 point, leading to a stratification of patients into three different prognostic groups: low risk (score 0-1), intermediate risk (2-3), and high risk (score 4), according to a report published online in Leukemia Research.
According to Stefano Molica, MD, of the Azienda Ospedaliera Pugliese-Ciaccio, Catanzaro, Italy, and his colleagues, the majority of patients (82%) were clinical Rai stage II-IV. The median patient age was 63 years and nearly 68% were men.
The researchers assessed four models for predicting overall survival. The modified version of CLL-International Prognostic Index (CLL-IPI) failed to provide prognostic information in relapsed/refractory (R/R) CLL (P = .77) as did the Ahn et al. model (P = .95) and a simplified BALL model (P = .09). In contrast, the full BALL score captured two groups of patients with significant differences in survival (hazard ratio, 0.240; 95 % confidence interval, 0.10-0.54; P = .0005); however, because of the low number of patients in the high-risk category, these cases were combined with the intermediate-risk group.
The BALL score identified a subset of patients, accounting for about 50% of the whole population, who particularly benefit from single-agent ibrutinib, according to Dr. Molica and his colleagues. These patients had a survival rate of 85% at 3 years.
“In contrast, the outcome of subjects with intermediate-high risk is disappointing. These patients should be considered for a combination of targeted drugs or cellular-based therapies,” the researchers concluded.
Cohen Expands on Treatment Options in Patients With Genomic Aberrations in CLL
Cohen Expands on Treatment Options in Patients With Genomic Aberrations in CLL
This article was originally published by Targeted Oncology
During a virtual Case Based Peer Perspective event, Jonathon B. Cohen, MD, MS, the codirector of the Lymphoma Program, medical director of Infusion Servies, and associate professor in the Department of Hematology and Medical Oncology at Emory University School of Medicine and Winship Cancer Institute, discussed a case of a 71-year-old woman diagnosed with chronic lymphocytic leukemia.
Targeted Oncology™: What are reasonable treatment options to consider in a patient with CLL?
COHEN: The National Comprehensive Cancer Network guidelines offer 6 treatment options for patients with del(17p).1 As I tell my fellows when I work with them, if you ever see a list of preferred regimens with 6 options, that likely means that nobody really knows what the best option is.
The 1 option not listed in the guideline is chemotherapy, especially in the relapsed setting for patients with del(17p). I generally would not use chemotherapy.
The only exception to that might be a situation where we have a patient who’s young and for whom we’re thinking about moving on to something like an allogeneic transplant or some other definitive therapy. We might consider using chemotherapy for a cycle or 2. But otherwise, if you’re not going in that direction, that’s the 1 thing we do feel comfortable saying—that is, that chemotherapy is probably not the right option.
FDA Clears clonoSEQ to Detect MRD in Chronic Lymphocytic Leukemia
FDA Clears clonoSEQ to Detect MRD in Chronic Lymphocytic Leukemia
This article was originally published by AJMC
Adaptive Biotechnologies received its third approval from the FDA for the use of its next-generation sequencing assay to detect minimal residual disease (MRD) in chronic lymphocytic leukemia (CLL).
The assay, clonoSEQ, uses a proprietary immunosequencing platform to monitor for MRD, where a small number of cancer cells remain during and after treatment. It is difficult to detect without precise, sensitive tools, and can lead to a recurrence of disease.
The approval follows a decision by CMS in January to pay for cloneSEQ testing for CLL, in addition to multiple myeloma and B-cell acute lymphoblastic leukemia. Nearly 80% of US patients with CLL are age 65 or over.
Continue reading this article on AJMC
Experts Outline Best Practices in the Treatment of Chronic Lymphocytic Leukemia
Experts Outline Best Practices in the Treatment of Chronic Lymphocytic Leukemia
This article was originally published by Pharmacy Times
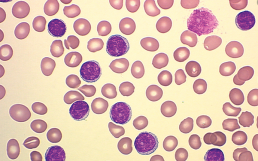
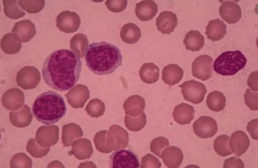
Chronic lymphocytic leukemia (CLL) is a cancer of the blood and bone marrow that can be treated to extend the life of some patients even by decades. Treatments and best practices are developing rapidly and health care providers need to stay up to date on all relevant information. In a Pharmacy Times Insights video series, a panel of experts discussed how to best treat and monitor patients living with CLL.
The panel included Alison Duffy, PharmD, BCOP, an associate professor and clinical pharmacy specialist in oncology at the University of Maryland School of Pharmacy and Cody Steeves, PharmD, BCOP, a clinical pharmacist for Biologics by McKesson.
Both intravenous (IV) and oral CLL medications are available, each with their own benefits and disadvantages. A combination method is also used by many patients, but that also presents a unique set of challenges.
“Some of the economic challenges we’ve seen have been the timely approval of the oral and the IV therapy together because of pharmacy benefits and medical benefits, and so that can be a challenge, especially if a patient’s disease is very aggressive. If they have progressed on ibrutinib it would be really important to start their subsequent therapy very quickly, or it can progress to Richter transformation,” Duffy said. “The economic challenges in improving can be a barrier. As pharmacists, anything we can do to facilitate the approval process, and in the clinic, I can certainly help with the prior authorization process.”