The Role of Chemoimmunotherapy Dwindles Among New Regimens in Frontline CLL
The Role of Chemoimmunotherapy Dwindles Among New Regimens in Frontline CLL
This article was originally published by OncLive
Although frontline chemoimmunotherapy regimens have been the gold standard for patients with chronic lymphocytic leukemia (CLL) for many years, the advent of BTK inhibitors and other novel drugs has moved the field toward adopting chemotherapy-free options for patients in this setting.
“For 50 years or so, there weren’t too many major developments in this field,” said Matthew S. Davids, MD, MMSc, director of clinical research and the lymphoma program at Dana-Farber Cancer Institute. “We had some improvements in the intensity of chemoimmunotherapy regimens, but in the last 10 years, we have had some really remarkable developments where the whole field was transformed.”
In an virtual presentation during the 2nd Annual Precision Medicine Symposium, a program developed by Physicians’ Education Resource® LLC, Davids, who is also an associate professor of medicine at Harvard Medical School, discussed the switch to chemotherapy-free regimens and whether chemoimmunotherapy combinations will retain a role in the frontline treatment of patients with CLL.
Novel Therapies Challenge Standard Frontline Chemoimmunotherapy Regimens
Upfront fludarabine, cyclophosphamide, and rituximab (Rituxan; FCR) chemoimmunotherapy was considered the gold standard for patients with CLL. Moreover, studies such as the FCR 300 and CLL8 trials showed that time-limited FCR can provide functional cure in patients with IGHV-mutant CLL.1,2
“This does highlight the important role of IGHV mutation status when we are thinking about using chemoimmunotherapy,” explained Davids. “IGHV-unmutated patients tend to have steady disease progression over time and do not enjoy the potential functional cure [that IGHV-mutated patients may derive].”
Other chemoimmunotherapy regimens such as bendamustine and rituximab (BR), which is widely used in the community setting, according to Davids, and obinutuzumab (Gazyva) plus chlorambucil, are also active in the frontline CLL space.
However, in recent years, studies have demonstrated superiority with novel regimens compared with chemoimmunotherapy.
“Much of [the advancements made in CLL] are due to the investment in basic science that was done in the late 1990s and early 2000s that allowed us to understand the role of the microenvironment in CLL and how that can be leveraged to treat the disease,” said Davids.
For example, in the phase 3 ECOG 1912 trial, the combination of the BTK inhibitor ibrutinib (Imbruvica) and rituximab, followed by ibrutinib maintenance therapy, demonstrated favorable progression-free survival (PFS) compared with FCR chemoimmunotherapy in patients 70 years or younger with previously untreated CLL.3
At a median follow-up of 33.6 months, the PFS rate was 89.4% with the ibrutinib/rituximab regimen versus 72.9% with chemoimmunotherapy (HR, 0.35; 95% CI, 0.22-0.56; P < .001). Moreover, overall survival (OS) also favored the chemotherapy-free regimen at 98.8% versus 91.5% with chemoimmunotherapy (HR, 0.17; 95% CI, 0.05-0.54; P < .001).
However, at 3 years, the PFS rate in patients with IGHV-mutant disease was 87.7% with ibrutinib/rituximab versus 88% with FCR (HR, 0.44; 95% CI, 0.14-1.36).
Although these chemotherapy-free options have been revolutionary in the frontline treatment of patients with CLL, chemoimmunotherapy may still be considered in this particular subgroup of IGHV-mutant patients, according to Davids.
“For my young fit patients with IGHV-mutant disease, FCR is certainly still part of the conversation,” Davids explained, adding that data suggest BR and obinutuzumab/chlorambucil are also options for these patients. In particular, BR should be considered for older, frail, IGHV-mutant patients who have cardiovascular comorbidities since giving BTK inhibitor therapy could increase the risk of cardiovascular events.
Similarly, results from the randomized phase 3 ELEVATE-TN trial demonstrated that acalabrutinib (Calquence) with or without obinutuzumab significantly improved PFS over obinutuzumab/chlorambucil chemoimmunotherapy.4 The median PFS at 28.3 months of follow-up was not reached with acalabrutinib as monotherapy or in combination with obinutuzumab versus 22.6 months with chemoimmunotherapy (HR, 0.1; 95% CI, 0.06-0.17; P < .0001; HR 0.20; 95% CI, 0.13-0.30; P < .0001).
Moreover, Davids added, chemoimmunotherapy may be selected in patients who prefer a time-limited therapy versus continuous treatment with a newer regimen.
“We can give 6 months of FCR and know that we have a good chance of very long-term remission,” said Davids. “We do have to counsel patients about cytopenias, infection risk, and secondary myeloid neoplasms. [These] are slightly more common in patients with CLL treated with FCR, but the rates are low.”
CLL14 Trial Aims to Eliminate the Need for Chemotherapy Altogether
The extended follow-up from the phase 3 CLL14 trial showed that the estimated 24-month PFS rate was 88.2% with the combination of venetoclax (Venclexta) and obinutuzumab versus 64.1% with obinutuzumab/chlorambucil.5 Although there was no statistically significant difference in OS between arms, venetoclax/obinutuzumab was associated with a low incidence of high-grade adverse effects in patients with relevant comorbidities.
CLL Advocates NZ Newsletter Issue 4
CLL Advocates NZ Newsletter Issue 4
Friends of CLL Advocates NZ
This month is Blood Cancer Awareness Month, so it was a good opportunity to reflect on collaboration, networking, and resource sharing between CLL Advocates New Zealand and other blood cancer patient support groups, which like us, are working to better understand and treat these disorders, and support those with them.
A recent and significant example of this is a current, and near complete, project of launching our ‘CLL Guide for Patients’ booklet. We have worked with and drawn upon the resources of Leukaemia Care, a national UK blood cancer support charity, to adapt their patient booklet for a New Zealand CLL setting. Within the next month CLLANZ will be launching this CLL patient guide. Leukaemia and Blood Cancer NZ (LBC) will also be launching an updated version of their own CLL booklet.
Education and learning are a major part of the way forward in your CLL journey, so I encourage you to access a copy of our booklet, which will be available in both hard copy and as a PDF download on our website. I’m sure you will find it an informative resource.
A lot of work has gone into the CLLANZ booklet, and I would like to thank Dr Gillian Corbett, Catherine Isaac, and Heather Phillips for their great work in putting the document together.
Following on from education and learning, the CLLANZ inaugural patient seminar is this coming month. Three of NZ’s experts on CLL will speak, followed by a panel discussion and questions. This is a joint event with LBC, at the LBC headquarters in Auckland, or on Zoom from anywhere, to be held on Wednesday 14 October. Registration and details can be found on our website here.
In support of other CLL patient support groups, I want to remind you of the resources and networking available globally including groups such as PatientPower and HealthUnlocked. These websites have a lot of useful information and their patient networks, while in a global setting, are very active. You can join the HealthUnlocked global community here, which boasts just under 16,000 members, and access the PatientPower CLL online events here.
There are also regular teleconferences, and other educational activities, which we have now started listing on our website here in a new events section. Many of these events are international webinars held at difficult times of the day for most of us here in New Zealand. So, we are working to access recordings of these to share with you to watch on-demand.
Another CLL group was also recently formed – Doctors with CLL, which I have joined. I will keep you posted on developments here. The umbrella organisation is CLLAN (CLL Advocates Network), based in Europe, and the organisers of the conference I attended in Edinburgh a year ago. CLLAN coordinates the activities of these groups, and there is a lot of information on their website.
There are a number of other activities also underway that I have shared recently, and which you hopefully you have in your diaries:
- Survey on participation in drug trials.
- Dr Karen Oldfield’s PhD research project questionnaire on medical marijuana use in NZ.
- Shared experiences within our group, of second malignancies that they have had in addition to their CLL.
Thank you to all of you who have been posting and engaging with material on our Private Facebook Group. Engagement from patients and supporters helps others feel confident about sharing their own stories, struggles and questions, so I encourage you to please use this platform to share resources, ask questions and comment and engage with one another. This activity will go on to help us grow the group.
Finally, the general election is this coming month. An important issue for CLL patients is funding of medications. I encourage you to look at the health policies of the significant parties and put attention on their position on Pharmac funding. A good website to look at all parties and their policies all at once is www.policy.nz. You can link directly to the health funding policies here.
Best wishes
Neil Graham
Triple Therapy for CLL Shows Promise in Phase 2 Trial
Triple Therapy for CLL Shows Promise in Phase 2 Trial
This article was originally published by Cancer Therapy Advisor
Results from a phase 2 study of 3 oral targeted agents for chronic lymphocytic leukemia (CLL) showed that patients achieved deep remissions after a limited-time duration treatment. The study, published in the Journal of Clinical Oncology, included both treatment-naive patients and those with recurrent/relapsed disease.1 The regimen worked well enough that phase 3 studies are underway.
Patients in this trial (ClinicalTrials.gov Identifier: NCT02427451) received a combination regimen of obinutuzumab, ibrutinib, and venetoclax.2 The 3 agents have different mechanisms of action, and are thought to combine well against CLL. Obinutuzumab, an anti-CD20 monoclonal antibody, is given first, followed by ibrutinib, which inhibits the B-cell signaling protein Bruton tyrosine kinase (BTK). Venetoclax, a BCL-2 inhibitor, comes last.
“We took the 3 most highly effective nonchemotherapy drugs that we had in CLL, put them in this regimen, and dosed them so they’re started sequentially,” said the study’s lead investigator Kerry Rogers, MD, hematologist with The Ohio State University Comprehensive Cancer Center’s Arthur G. James Cancer Hospital and Richard J. Solove Research Institute in Columbus.
The CLLANZ Inaugural CLL Seminar
CLLANZ Inaugural Patient Seminar
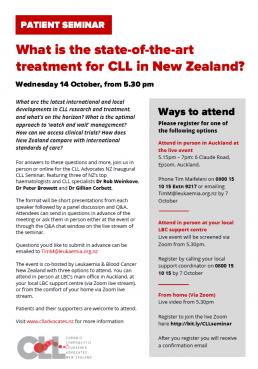
What is the state-of-the-art treatment for CLL in New Zealand?
What are the latest international and local developments in CLL research and treatment, and what’s on the horizon? What is the optimal approach to ‘watch and wait’ management? How can we access clinical trials? How does New Zealand compare with international standards of care?
For answers to these questions and more, join us in person or online for the CLL Advocates NZ Inaugural CLL Seminar, featuring three of NZ’s top haematologists and CLL specialists Dr Rob Weinkove, Dr Peter Browett and Dr Gillian Corbett.
The format will be short presentations from each speaker followed by a panel discussion and Q&A. Attendees can send in questions in advance of the meeting or ask them in person either at the event or through the Q&A chat window on the live stream of the seminar. Questions you’d like to submit in advance can be emailed to TimM@leukaemia.org.nz
The event is co-hosted by Leukaemia & Blood Cancer New Zealand with three options to attend.
You can attend in person at LBC’s main office in Auckland, at your local LBC support centre (via Zoom live stream), or from the comfort of your home via Zoom live stream. See details below.
Patients and their supporters are welcome to attend. Please register for one of the following.
Presentations
Options to attend
Attend in person in Auckland at the live event
5.15pm – 7pm: 6 Claude Road, Epsom, Auckland
Register by phoning Tim Maifeleni on 0800 15 10 15 Extn 9217 or emailing TimM@leukaemia.org.nz by 7 October
Attend in person at your local LBC support centre
Live event will be screened via Zoom from 5.30pm
Register by calling your local support coordinator on 0800 15 10 15 or email info@leukaemia.org.nz by 7 October
From home (Via Zoom)
Live video from 5.30pm
Register to join the live Zoom meeting here
After you register you will receive a confirmation email
Uncommon Mutation in CLL Associated With More Favorable Prognostic Factors
Uncommon Mutation in CLL Associated With More Favorable Prognostic Factors
This article was originally published by Cancer Therapy Advisor
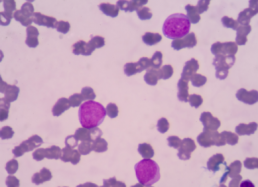
Patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) who had an MYD88 L265P mutation were uncommon and had distinct features, reported a cohort study in Blood Cancer Journal.
Study researchers identified 56 (3.1%) patients with CLL/SLL who had MYD88 mutations among 1779 who underwent mutational analysis. The study also included 100 patients who did not have MYD88 mutations to serve as a control group.
Among patients with MYD88 mutations, 38 (68%) had the L265P mutation and 18 (32%) had non-L265P mutations, which included 10 with V217F and 4 with M232T. Among the remaining patients with non-L265P mutations, 2 had a single-nucleotide mutation, 1 with S219C and the other with A6fs, and 2 had concurrent mutations, 1 with N291S/T294P and the other with F252I/M232T.
No morphological differences were seen, as all patients had a typical CLL morphology. In general, patients with non-L265P mutations had similar features to patients with wild-type MYD88.
Targeted Molecular Therapies for the Treatment of Chronic Lymphocytic Leukemia
Targeted Molecular Therapies for the Treatment of Chronic Lymphocytic Leukemia
This article was originally published by Hematology Advisor
Chronic lymphocytic leukemia (CLL) presents as an accumulation of monoclonal, mature, CD5+ B-cells in secondary lymphatic organs where cancer cells engage in molecular and cellular interactions disrupting the adaptive immune response. Promising advances in therapy options for patients with CLL, targeting these molecular interactions, were discussed in a review published in The New England Journal of Medicine.1
Since the introduction of these novel therapeutics, the use of chemoimmunotherapy has drastically declined. “We have moved away from using chemotherapy for most patients, just over the last 5 years”, Jan Burger, MD, PhD, of the department of leukemia at the University of Texas MD Anderson Cancer Center in Houston, told Hematology Advisor.
“We now have good alternatives to chemotherapy that, in the end, have better survival rates for our patients” Dr Burger, who is the author of the review paper, continued. “The reason why we were able to make this big step forward in treatment was to some extent [serendipitous]. These new kinase inhibitors became available at a time when there was more basic research which emphasized how important these molecules are in leukemia cells.”
Which Drug Therapy for CLL, Time-Limited or Continuous?
Which Drug Therapy for CLL, Time-Limited or Continuous?
This article was originally published by Medscape
About two thirds of patients who are diagnosed with chronic lymphocytic leukemia (CLL) are initially managed with a ‘watch-and-wait’ approach, but other one third of patients will need to be started on drug therapy straight away. But with which regimen?
The standard therapy to date has been time-limited chemoimmunotherapy, and this still has a key role to play in certain cases. But evolving continuous treatments and evidence on the array of factors that can influence response are making decision-making more individualized than ever, said Matthew S. Davids, MD, MMSc, director of clinical research in the Division of Lymphoma at Dana-Farber Cancer Institute and associate professor of medicine at Harvard Medical School, Boston, Massachusetts.
“Continuous versus time-limited treatment discussions are long discussions now and should be individualized to particular patients and their comorbidities,” said Davids.
Davids was speaking at a “How I Treat” session at the recent American Society of Hematology’s (ASH) Meeting on Hematological Malignancies, which was held virtually because of the COVID-19 pandemic.
Key Factors to Consider
Key factors in determining the most effective approach are the patient’s TP53 and immunoglobulin heavy chain (IGHV) gene mutation status, Davids said.
For instance, the traditional choice for frontline care for CLL has been standard chemoimmunotherapy (eg, fludarabine, cyclophosphamide and rituximab [FCR]), with a typical treatment duration of 6 months. However, the response effects appear most durable in younger patients with mutated IGHV and intact TP53.
As evidence, Davids cited data from a long-term follow-up of one of the original FCR studies in 300 patients, which found that about 60% of patients had long-term disease-free survival.
EU approves Imbruvica plus rituximab in first-line CLL
EU approves Imbruvica plus rituximab in first-line CLL
This article was originally published by The Pharma Letter
Johnson & Johnson (NYSE: JNJ) and AbbVie (NYSE: ABBV) have secured approval for a broader label for the BTK blocker Imbruvica (ibrutinib) in Europe.
The decision extends the approved indication in chronic lymphocytic leukemia (CLL) to include first-line treatment in combination with the targeted biologic therapy rituximab, and comes months after the US regulator provided approval in the same indication.
The decision is based on data from the Phase III E1912 study, which provides a favorable comparison with the established chemo-immunotherapy regimen fludarabine, cyclophosphamide and rituximab (FCR).
Profitable partnership
First approved in 2013, Chicago-based AbbVie (NYSE: ABBV) is jointly developing and commercializing Imbruvica with J&J’s pharma arm, Janssen.
The firms are in an equal partnership in developing the drug, after AbbVie acquired the original development partner Pharmacyclics for $21 billion in 2015.
The new approval in CLL represents the 11th approval overall for the product, and the sixth approval for Imbruvica in this cancer type.
4 October - CLL Treatments Today: What Should I Know?
Online webinar: CLL Treatments Today: What Should I Know?
Virtual town meeting - 4 October 5am (NZST)
Overview
Join this virtual town meeting for chronic lymphocytic leukemia (CLL) patients and family members on Saturday, October 3, 2020 starting at 9 am PT/12 pm ET. This 3-hour program will take you through a CLL 101, 201 and 301 class hosted by CLL patient advocates and experts from Cleveland Clinic and University Hospitals Cleveland Medical Center. All attendees will receive a special Powerful Patient face mask.
We want you to be part of this event! Send us your best selfie, or a picture of you with your family, or a pet –anything that tells us who you are! You might just see it on the screen! Please send it to cll@patientpower.info. By sending it to us, you consent to its use in the CLL town hall recorded content and live stream.
Agenda
12:00-12:30 pm ET- CLL 101 – Information for the newly diagnosed. Learn about the stages of CLL, how to talk to your friends and family, and what to ask your doctor.
12:30-12:45 pm ET- CLL and COVID-19 – Is it safe to start or resume treatment right now? Find out how the coronavirus pandemic is impacting CLL patients.
12:45- 1:30 pm ET- CLL 201 – Learn about the current CLL landscape, including treatment options, side effects and the significance of minimal residual disease (MRD) testing.
1:30-1:45 pm ET – Break
1:45 -2:30 pm ET- CLL 301 – Experts discuss the future of CLL treatment, including FDA approvals, clinical trials and Richter’s Transformation.
2:30-3 pm ET – Q&A
Clinical Trials Survey 2020
Clinical Trials Survey 2020
Andrew Schorr, Patient Power co-founder, is the virtual keynote speaker to hundreds of people who supervise cancer clinical trials. The event is on September 10th. The event organizers want Andrew to share his perspective – and yours – on participation in cancer clinical trials now, during the time of the pandemic.
Please help Andrew give a powerful speech based on your experiences and thoughts around clinical trials in context of Covid-19.
The survey will just take a couple of minutes of your time. Thanks for helping and feel free to share with other patients!