Novel Prognostic Model Predictive of Survival in Ibrutinib-Treated CLL
Novel Prognostic Model Predictive of Survival in Ibrutinib-Treated Chronic Lymphocytic Leukemia
This article was originally published by Hematology Advisor
A 4-factor prognostic model may help to identify patients with chronic lymphocytic leukemia (CLL) at risk of ibrutinib failure, according to research published in the Journal of Clinical Oncology.
As CLL is a “clonal expansion of mature B cells drive by constitutive activation of B-cell receptor (BCR) signaling,” previous studies suggest that the selective inhibition of BCR and BCL-2 protein may significantly improve outcomes in some patients with CLL compared with chemotherapy as a first-line therapy.
Ibrutinib, a Bruton tyrosine kinase inhibitor, is frequently used in the CLL setting, though drug resistance invariably evolves, with relapse occurring often with ibrutinib monotherapy.
Identifying those at risk of relapse after ibrutinib therapy would improve treatment decision-making among patients with CLL. While there are existing prognostic indices, none specifically evaluate for criteria known to be linked with the evolution of ibrutinib resistance. In the present study, the researchers evaluated and validated the effectiveness of a 4-factor prognostic model among patients with CLL treated with ibrutinib.
CLL Advocates NZ Launches a New Zealand Patient Guide
CLL Advocates NZ Launches a New Zealand Patient Guide
CLL Advocates NZ is pleased to announce the official launch of its patient booklet, CLL – A Guide for Patients in New Zealand. It has been made available in both a digital download and as a hardcopy booklet.
The booklet is being launched at CLL Advocates NZ’s inaugural patient seminar in Auckland and online tonight (14 October). The seminar will discuss ‘What is the state-of-the-art treatment for CLL in New Zealand?’
The booklet was compiled by Leukaemia Care, a national UK blood cancer support charity. Leukaemia Care has kindly granted us permission to adapt the booklet for the New Zealand CLL setting, and to publish it here on our website, and make it available as a printed booklet for distribution in New Zealand. This agreement is in line with CLL Advocates NZ’s commitment to working closely with other CLL patient advocacy groups and to avoid duplicating available high quality work undertaken by others.
Adaptation of the booklet for New Zealand conditions has been undertaken by Gillian Corbett MBChB, FRACPath, MRCP, FRACP, haematologist and Trustee, CLL Advocates NZ, Neil Graham FRACP, FRCP, Executive Director, CLL Advocates NZ, and Catherine Isaac, Trustee, CLL Advocates NZ.
We are most grateful to Leukaemia Care for this very valuable contribution to our work.
To learn more about the booklet, download it, or to request a hardcopy click here.
CLL Advocates NZ Newsletter Issue 4
CLL Advocates NZ Newsletter Issue 4
Friends of CLL Advocates NZ
This month is Blood Cancer Awareness Month, so it was a good opportunity to reflect on collaboration, networking, and resource sharing between CLL Advocates New Zealand and other blood cancer patient support groups, which like us, are working to better understand and treat these disorders, and support those with them.
A recent and significant example of this is a current, and near complete, project of launching our ‘CLL Guide for Patients’ booklet. We have worked with and drawn upon the resources of Leukaemia Care, a national UK blood cancer support charity, to adapt their patient booklet for a New Zealand CLL setting. Within the next month CLLANZ will be launching this CLL patient guide. Leukaemia and Blood Cancer NZ (LBC) will also be launching an updated version of their own CLL booklet.
Education and learning are a major part of the way forward in your CLL journey, so I encourage you to access a copy of our booklet, which will be available in both hard copy and as a PDF download on our website. I’m sure you will find it an informative resource.
A lot of work has gone into the CLLANZ booklet, and I would like to thank Dr Gillian Corbett, Catherine Isaac, and Heather Phillips for their great work in putting the document together.
Following on from education and learning, the CLLANZ inaugural patient seminar is this coming month. Three of NZ’s experts on CLL will speak, followed by a panel discussion and questions. This is a joint event with LBC, at the LBC headquarters in Auckland, or on Zoom from anywhere, to be held on Wednesday 14 October. Registration and details can be found on our website here.
In support of other CLL patient support groups, I want to remind you of the resources and networking available globally including groups such as PatientPower and HealthUnlocked. These websites have a lot of useful information and their patient networks, while in a global setting, are very active. You can join the HealthUnlocked global community here, which boasts just under 16,000 members, and access the PatientPower CLL online events here.
There are also regular teleconferences, and other educational activities, which we have now started listing on our website here in a new events section. Many of these events are international webinars held at difficult times of the day for most of us here in New Zealand. So, we are working to access recordings of these to share with you to watch on-demand.
Another CLL group was also recently formed – Doctors with CLL, which I have joined. I will keep you posted on developments here. The umbrella organisation is CLLAN (CLL Advocates Network), based in Europe, and the organisers of the conference I attended in Edinburgh a year ago. CLLAN coordinates the activities of these groups, and there is a lot of information on their website.
There are a number of other activities also underway that I have shared recently, and which you hopefully you have in your diaries:
- Survey on participation in drug trials.
- Dr Karen Oldfield’s PhD research project questionnaire on medical marijuana use in NZ.
- Shared experiences within our group, of second malignancies that they have had in addition to their CLL.
Thank you to all of you who have been posting and engaging with material on our Private Facebook Group. Engagement from patients and supporters helps others feel confident about sharing their own stories, struggles and questions, so I encourage you to please use this platform to share resources, ask questions and comment and engage with one another. This activity will go on to help us grow the group.
Finally, the general election is this coming month. An important issue for CLL patients is funding of medications. I encourage you to look at the health policies of the significant parties and put attention on their position on Pharmac funding. A good website to look at all parties and their policies all at once is www.policy.nz. You can link directly to the health funding policies here.
Best wishes
Neil Graham
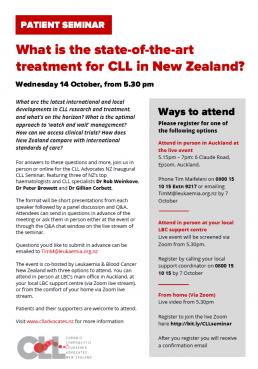
The CLLANZ Inaugural CLL Seminar
CLLANZ Inaugural Patient Seminar
What is the state-of-the-art treatment for CLL in New Zealand?
What are the latest international and local developments in CLL research and treatment, and what’s on the horizon? What is the optimal approach to ‘watch and wait’ management? How can we access clinical trials? How does New Zealand compare with international standards of care?
For answers to these questions and more, join us in person or online for the CLL Advocates NZ Inaugural CLL Seminar, featuring three of NZ’s top haematologists and CLL specialists Dr Rob Weinkove, Dr Peter Browett and Dr Gillian Corbett.
The format will be short presentations from each speaker followed by a panel discussion and Q&A. Attendees can send in questions in advance of the meeting or ask them in person either at the event or through the Q&A chat window on the live stream of the seminar. Questions you’d like to submit in advance can be emailed to TimM@leukaemia.org.nz
The event is co-hosted by Leukaemia & Blood Cancer New Zealand with three options to attend.
You can attend in person at LBC’s main office in Auckland, at your local LBC support centre (via Zoom live stream), or from the comfort of your home via Zoom live stream. See details below.
Patients and their supporters are welcome to attend. Please register for one of the following.
Presentations
Options to attend
Attend in person in Auckland at the live event
5.15pm – 7pm: 6 Claude Road, Epsom, Auckland
Register by phoning Tim Maifeleni on 0800 15 10 15 Extn 9217 or emailing TimM@leukaemia.org.nz by 7 October
Attend in person at your local LBC support centre
Live event will be screened via Zoom from 5.30pm
Register by calling your local support coordinator on 0800 15 10 15 or email info@leukaemia.org.nz by 7 October
From home (Via Zoom)
Live video from 5.30pm
Register to join the live Zoom meeting here
After you register you will receive a confirmation email
4 October - CLL Treatments Today: What Should I Know?
Online webinar: CLL Treatments Today: What Should I Know?
Virtual town meeting - 4 October 5am (NZST)
Overview
Join this virtual town meeting for chronic lymphocytic leukemia (CLL) patients and family members on Saturday, October 3, 2020 starting at 9 am PT/12 pm ET. This 3-hour program will take you through a CLL 101, 201 and 301 class hosted by CLL patient advocates and experts from Cleveland Clinic and University Hospitals Cleveland Medical Center. All attendees will receive a special Powerful Patient face mask.
We want you to be part of this event! Send us your best selfie, or a picture of you with your family, or a pet –anything that tells us who you are! You might just see it on the screen! Please send it to cll@patientpower.info. By sending it to us, you consent to its use in the CLL town hall recorded content and live stream.
Agenda
12:00-12:30 pm ET- CLL 101 – Information for the newly diagnosed. Learn about the stages of CLL, how to talk to your friends and family, and what to ask your doctor.
12:30-12:45 pm ET- CLL and COVID-19 – Is it safe to start or resume treatment right now? Find out how the coronavirus pandemic is impacting CLL patients.
12:45- 1:30 pm ET- CLL 201 – Learn about the current CLL landscape, including treatment options, side effects and the significance of minimal residual disease (MRD) testing.
1:30-1:45 pm ET – Break
1:45 -2:30 pm ET- CLL 301 – Experts discuss the future of CLL treatment, including FDA approvals, clinical trials and Richter’s Transformation.
2:30-3 pm ET – Q&A
Clinical Trials Survey 2020
Clinical Trials Survey 2020
Andrew Schorr, Patient Power co-founder, is the virtual keynote speaker to hundreds of people who supervise cancer clinical trials. The event is on September 10th. The event organizers want Andrew to share his perspective – and yours – on participation in cancer clinical trials now, during the time of the pandemic.
Please help Andrew give a powerful speech based on your experiences and thoughts around clinical trials in context of Covid-19.
The survey will just take a couple of minutes of your time. Thanks for helping and feel free to share with other patients!
Online webinar: Telling Others About My CLL Diagnosis
Online webinar: Telling Others About My CLL Diagnosis
How do you tell family and friends that you have leukemia? Chronic Lymphocytic Leukemia (CLL) patients often don’t “look sick” so it may be hard for your family, friends and co-workers to know what you are going through. How do you help others understand your condition?
Join us for our next CLL Answers Now program on Wednesday, September 16th at 10:30 am PT/1:30 pm ET as host and CLL patient Michele Nadeem-Baker discusses with social worker Robin Katz from Lurie Cancer Center of Northwestern University communication tips for people living with CLL, and the best way to share details of their condition. They will also discuss how to talk to their loved ones about their diagnosis and give advice to people newly diagnosed.
Send your questions in ahead to cll@patientpower.info.
Wednesday, September 16, 2020 at 10:30 AM Pacific Time (US and Canada)
World Leukemia Day - 4 September 2020
World Leukemia Day - 4 September 2020
World Leukemia Day is on September 4th and we’d love you to join us.
We are looking for people from all around the globe to participate in increasing the awareness of leukemia that is so vital to help improve the lives of patients after diagnosis.
Here are 3 ways to get involved:
1. Share your leukemia story
Encourage others to share their leukemia story on social media and use the hashtags #WLD2020 or #WorldLeukemiaDay. More information is available at www.worldleukemiaday.org
2. Share your ‘spotty selfie’
Dig out your spotty clothes and share your ‘spotty selfie’ on social media with the hashtag #WLD20 on September 4th to show your support.
3. Spread the word
Help raise awareness of the symptoms of leukemia by using our social media graphics and sharing these across your social media platforms along with the hashtags #WLD20 #worldleukemiaday.
You can download all the social media graphics here > https://bit.ly/WorldLeukemiaDay
World Leukemia Day isn’t just about raising awareness, it’s also about education and learning how to spot the signs and symptoms. For some types of leukemia early diagnosis is crucial, if you are experiencing any of the symptoms, speak to a healthcare professional about your concerns.
Find out more about the signs and symptoms here > https://www.worldleukemiaday.org/what-is-leukemia
We look forward to seeing your ‘spotty selfies’ on September 4th.
Your CLL Advocates Network



CLL Advocates NZ Newsletter Issue 3
CLL Advocates NZ Newsletter Issue 3
Greetings
Research is a critical part of understanding diseases and their treatment. As set out in our Trust Deed, a key objective for CLL Advocates NZ is to ‘promote and support NZ-based research on CLL, including the value and importance of developing and participating in clinical trials, and improving the quality of NZ data on CLL. In pursuit of this objective we’re developing or supporting a number of initiatives:
- Clinical trials in NZ. You can find information on our website about ClinTrial Refer New Zealand. If you’re interested in keeping up to date with trials of CLL treatments in NZ, you can download the free app supported by HSANZ (Haematology Society of Australia and NZ) here. A number of New Zealanders have been enrolled in trials, often gaining access to unfunded medications, including “last resort” treatment options for advanced disease. There are numerous such trials actively recruiting as I write. One is Rob Weinkove’s work at the Malaghan Institute in Wellington, on CAR – T cell therapy. Trials of Zanubrutinib vs Ibrutinib are also recruiting in New Zealand.
- Second malignancies in CLL. We have proposed a summer studentship/research grant in the Bay of Plenty on this topic. Second malignancies are one of the commonest causes of death in CLL. They include Richter’s Syndrome and skin cancers, including melanoma. The project should start at the end of 2020. Having been a researcher in such studies myself, I know that patient involvement in research projects often significantly increases their own understanding of the disease, as they often involve frequent contact with health professionals and present good opportunities to talk about CLL with them.
- A PhD research study on the use of cannabis as a medicine for cancer patients. Dr Karen Oldfield is a PhD candidate at Victoria University of Wellington and a Senior Clinical Research Fellow at the Medical Research Institute of New Zealand, who is looking at the use of cannabis as a medicine in NZ. She’s inviting cancer patients to take part in a 5-10 minute online survey about their thoughts on this topic. All information collected will be treated as confidential. This is a valuable research project, as well as a way of fostering links between CLL patients and NZ research groups, and I warmly encourage you to take part. If you’re interested in helping with this research, go to this link on our website.
Finally, do remember the CLL forum we are having online and live at LBC headquarters on 14 October, 5.30 – 7.00pm. Invitations and details will be coming out shortly.
Best wishes
Neil Graham
Online webinar: Aggressive CLL Treatment Options: Are They Right for Me?
Online webinar: Aggressive CLL Treatment Options: Are They Right for Me?
How do experts decide when a CLL patient needs more aggressive treatments? In the age of oral therapy, when do CLL treatments such as CAR-T therapy and clinical trials make sense? Join us on Thursday, August 27th at 1 pm PT/4 pm ET for a live CLL Answers Now Program. Host Andrew Schorr will talk with University of Rochester Wilmot Cancer Center’s Dr. Paul Barr on these more aggressive treatment options for CLL. Please send questions in advance to cll@patientpower.info.
Thursday, August 27, 2020 at 1:00 PM Pacific Time (US and Canada)
CLLANZ will publish the link after the event has ended or you can register here